
Health system barriers and facilitators to living donor kidney transplantation: a tale of two states with the highest and lowest rates
Shaifali Sandal1, Anna Horton1, Katya Loban1, Peter Nugus1, Marcelo Cantarovich1, David Landsberg2, Michel Paquet3, Prosanto Chaudhury1, Marie-Chantal Fortin3.
1Nephrology, McGill University Health Centre, Montreal, QC, Canada; 2Nephrology, University of British Columbia, Vancouver, BC, Canada; 3Nephrology, University of Montreal, Montréal, QC, Canada
Purpose: Current efforts to increase living donor kidney transplantation (LDKT) entails identifying patient-level barriers and little is known about barriers that exist at the level of the health systems. The provision of transplantation in Canada is at the provincial level and there is wide variability in LDKT performance across different provinces. We aimed to learn and compare health systems with the best and the worst performance in LDKT, and to identify health system-level barriers to LDKT.
Methods: This study took the form of a comparative case study analysis. Case study research is an in-depth and non-interventional examination of a single case over time using retrospective and contemporary data. Data collection entailed semi-structured interviews, document review, and participant observation. Data were analyzed thematically to generate themes surrounding the attributes and processes of a health system that facilitate the delivery of LDKT to patients, and those that create barriers.
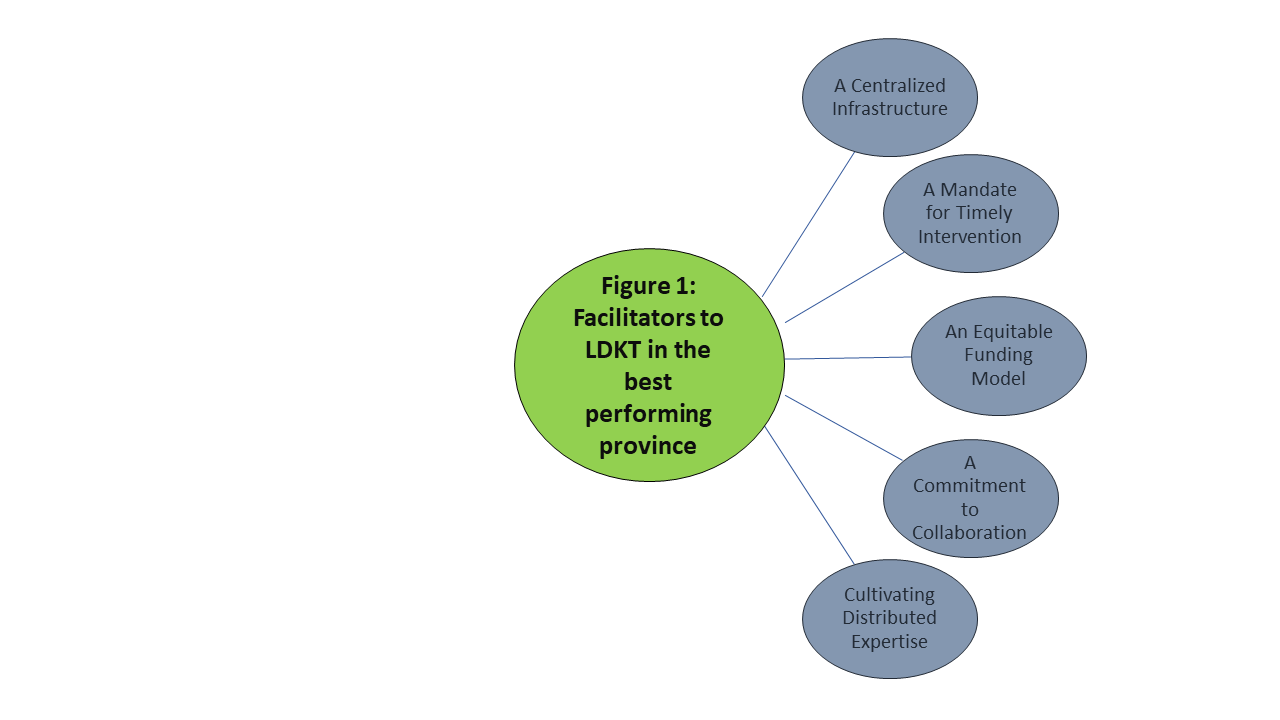
Results: In the best-performing province of Canada, five themes emerged as facilitators to the delivery of LDKT to patients. The relationship between two provincial organizations (a regional transplant and a regional nephrology order) was identified as key to enabling the mandate and processes for LDKT. On the other hand, in the worst-performing province, similar themes emerged as barriers to LDKT. Barriers were identified at the levels of organizational coordination, professional knowledge, resources, geography, and governance. Particularly, inconsistent coordination between regional clinics and transplant centers and poor role definition was seen to hinder and delay care processes.
Conclusion: By comparing two health systems with variable rates of LDKT, we have identified several real-world health system-level barriers to the delivery of LDKT to patients. Many of these barriers are modifiable and have implications for practitioners, policymakers, administrators, and patients.
This work is supported by a Gift of Life Institute Clinical Faculty Development Research Grant from the American Society of Transplantation and a Health Research Grant, Kidney Foundation of Canada.
