
Granulocyte colony-stimulating factor with or without immunosuppression reduction in neutropenic kidney transplant recipients
Shaifali Sandal1, Han Yao1, Ahsan Alam1, David D’Arienzo1, Dana Baran1, Marcelo Cantarovich1.
1Internal Medicine/Nephrology, McGill University Health Centre, Montreal, QC, Canada
Introduction: Neutropenia, defined as an absolute neutrophil count (ANC) of < 1,500/mm3, is a common complication after kidney transplantation (KT). It is associated with adverse graft and patient outcomes, yet little is known about the best management practices for neutropenia in transplant recipients. We aimed to analyze the effect of granulocyte colony-stimulating factor (G-CSF) use with and without immunosuppression reduction on graft outcomes in neutropenic KT recipients.
Methods: We conducted a retrospective cohort study of adult (age ≥18), deceased donor recipients of KT between September 1, 2011, and December 31, 2016, who developed neutropenia within the first-year post-KT. We excluded multiorgan transplant recipients, those who were undergoing re-KT, those with a history of HIV, or primary nonfunction. Clinically significant neutropenia was defined as 1) Two consecutive ANC of < 1500/mm3; or 2) One ANC value < 1500 cells/mm3 associated with a decrease in maintenance immunosuppression within 30 days of detection of neutropenia. Severe neutropenia was defined as an ANC < 500/mm3.
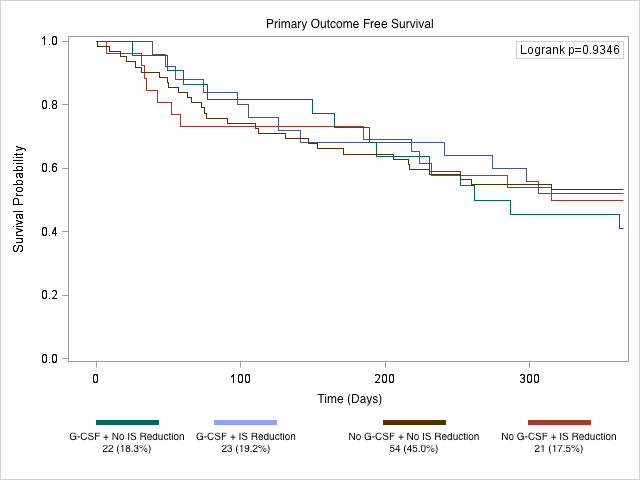
Results: We identified 120 recipients with neutropenia, within the first-year post-transplant. Of these, 45.0% underwent no intervention, 17.5% had immunosuppression reduced, 18.3% were only given G-CSF, and 19.2% had both interventions. Overall, 61 patients experienced the composite outcome of de-novo DSA, biopsy-proven acute rejection, and all-cause graft failure and the cumulative incidence of this outcome did not vary by any of the four interventions (p=0.93) (Figure). When stratifying the cohort by G-CSF use alone, those who received G-CSF were more likely to have had moderate (46.7% vs. 42.7%) or severe neutropenia (51.1% vs. 12.0%, p<0.001), and were more likely to have had immunosuppression reduction (51.1% vs. 28.0%, p=0.003). However, the composite outcome was not different in the G-CSF and no G-CSF cohort (53.3% vs. 49.3%, p=0.67), and in a multivariate model, G-CSF use was not associated with this outcome (aHR=1.18, 95%CI:0.61-2.30).
Conclusion: We conclude that G-CSF use with or without immunosuppression reduction was not associated with graft outcomes; however, this observation warrants prospective evaluation.
