
Analyzing the impact of the COVID-19 pandemic on communication and education strategies across transplant programs in Canada
Shaifali Sandal1, Elie Fadel1, Michael Gagnon1, Emilie Trinh1, Andrea Herrera-Gayol1, Marcelo Cantarovich1.
1Internal Medicine/Nephrology, McGill University Health Centre, Montreal, QC, Canada
Background: Effective communication and education strategies have been identified as key to increasing access to transplantation. The COVID-19 pandemic paradoxically accelerated the need to adopt virtual approaches. We aimed to compare communication and education strategies of Canadian transplant programs prepandemic and after March 2020 in order to develop a consensus on whether the pandemic led to better strategies.
Methods: We utilized the Delphi survey technique. First, via informal interviews and conversations, we created a short survey that was conducted from April to May 2019. Subsequently, we sent the same survey to the same participants from July to October 2021 but with the addition of two questions with the specific objective of determining whether the pandemic led to adopting better strategies; a priori consensus was defined as 75% of the participants agreeing/strongly agreeing or disagreeing with these statements. Links to both surveys were sent electronically, and participants were transplant physicians or surgeons in a leadership position at 60 solid organ transplant programs in Canada (20 pediatric and 40 adult).
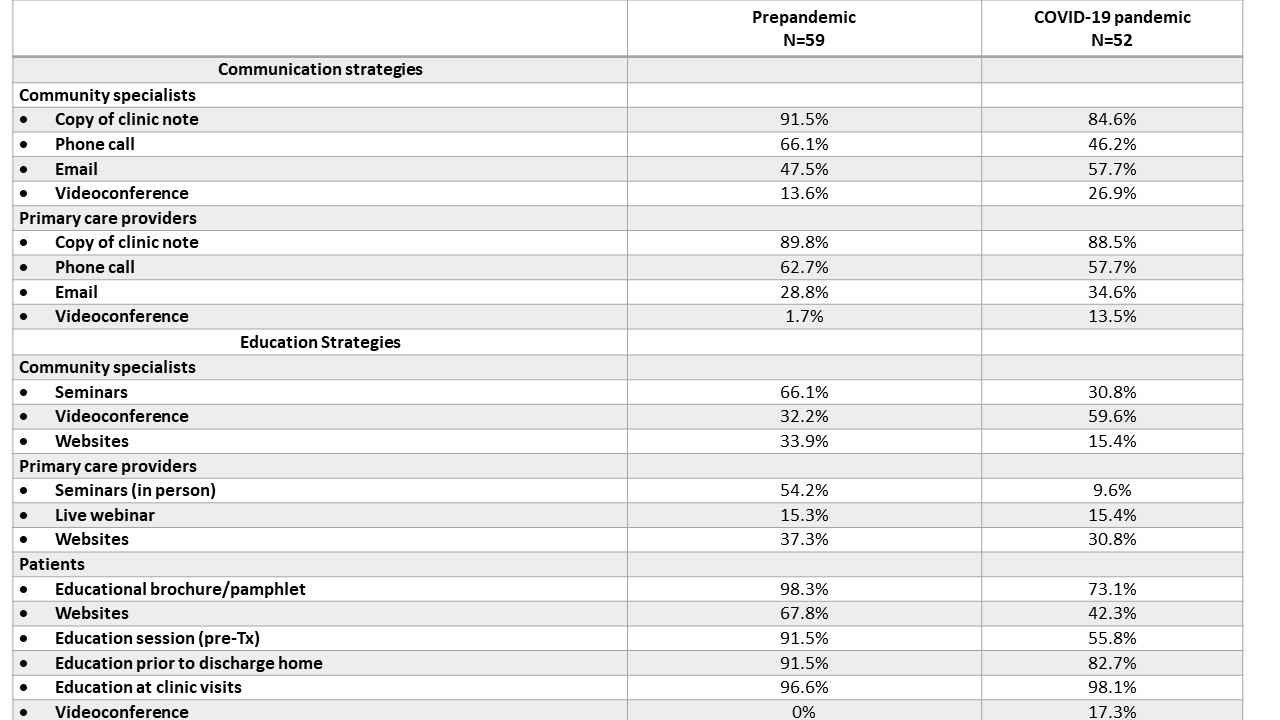
Results: The response rate for the first survey was 98.3% and for the second survey was 86.7%. As shown in Table 1, although the proportion of participants who selected videoconference as a communication strategy with community specialists, primary care providers, and patients increased substantially, the top choices remained clinic notes and in-person visits. However, there was a substantial decline in education strategies being used to educate community specialists, primary care providers, and particularly patients. Only 54% of participants agreed/strongly agreed with the statement “we developed better communication strategies during the pandemic” while 19.2% disagreed/strongly disagreed. Notably, 32.7% agreed/strongly agreed with the statement “we developed better education strategies during the pandemic” while 25.0% disagreed/strongly disagreed.
Discussion: Many transplant programs used traditional methods to communicate and educate patients, primary care providers, and community specialists prior to the pandemic. The COVID-19 pandemic did not lead to improvements in communication strategies and may have worsened education strategies in use by transplant programs. Despite the digitalization of several sectors, health care may lag in adopting effective virtual or telecommunication in clinical practice.
