
System-level barriers to living donor kidney transplantation: a cross-sectional survey study of health professionals
Shaifali Sandal1, Ian Schiller1, Nandini Dendukuri1, Jorane-Tiana Robert 1, Khaled Katergi1, Ahsan Alam1, Marcelo Cantarovich1, Julio F Fiore1, Rita Suri1, David Landsberg2, Catherine Weber1, Marie-Chantal Fortin3.
1Internal Medicine/Nephrology, McGill University Health Centre, Montreal, QC, Canada; 2Nephrology, University of British Columbia, Vancouver, BC, Canada; 3Internal Medicine/Nephrology, University of Montreal, Montreal, QC, Canada
Background and objectives: Living donor kidney transplantation (LDKT) is the preferred therapeutic option for patients with end-stage kidney disease and health professionals (HPs) can provide unique insights to improving the delivery of LDKT to patients. We aimed to quantify system-level barriers to LDKT that we have previously identified in our qualitative work and estimate their association with LDKT performance. We also aimed to determine if HP’s characteristics influenced responses and what HPs thought should be priorities to increase LDKT.
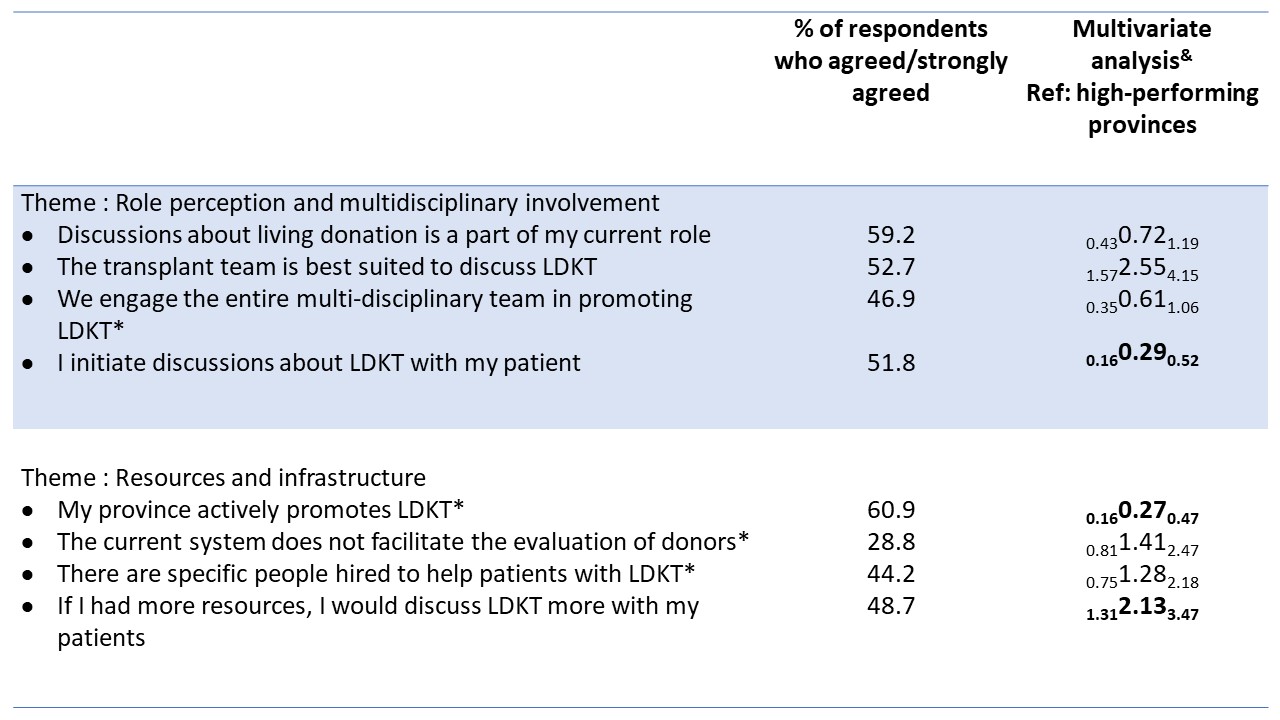
Methods: We conducted a cross-sectional survey of Canadian health professionals (HPs) and asked participants to rate statements on a Likert scale of 1-5 (strongly disagree-strongly agree). Statements captured themes related to communication, role perception, education/training/comfort, attitudes, referral process, patient as the barrier, and resources/infrastructure. The percentage of participants who agreed with these statements was analyzed and compared by LDKT performance (provincial living donation rates higher versus lower than the national average) and HP characteristics.
Results: We obtained 353 complete responses. Overall, themes related to poor communication, poor role perception and HPs education/training/comfort emerged as barriers to LDKT. When compared with HPs from high-performing provinces, those from low-performing provinces had lower odds of agreeing that their province promoted LDKT (aOR=0.27, 95%CI:0.16-0.48). They also had lower odds of initiating discussions about LDKT (aOR=0.30, 95%CI:0.17-0.55), higher odds of agreeing that the transplant team is best suited to discuss LDKT (aOR=2.64, 95%CI:1.60-4.33) and that more resources would increase LDKT discussions from them (aOR=2.06, 95%CI:1.25-3.40). When comparing responses by HP characteristics, non-physician role and <10 years of experience were associated with the level of agreement across several themes. Creating guidelines, streamlining evaluations, and improving communication were ranked as priorities to increase LDKT over patient education.
Conclusion: Poor communication between treating teams, poor role perception and HPs lack of education/training/comfort emerged as system-level barriers to LDKT and even HPs themselves identified addressing system-level inefficiencies as priorities to increase LDKT over patient education. More importantly, we report that poor role perception, low resources, and poor infrastructure may be driving differences in LDKT performance in a real-world setting. Our findings have policy implications and can build on the current patient-level work that others are pursuing to increase LDKT.
This work is supported by a Research Innovation Grant from the Canadian Donation and Transplant Research Program and 2021 Canada Summer Jobs competition from the Employment and Social Development of the Government of Canada.
