Survival after simultaneous pancreas‐kidney transplantation in type 1 diabetes: the critical role of early pancreas allograft function
Mengmeng Ji1, Mei Wang1, Wenjun Hu1, Mohamed Ibrahim1, Krista Lentine2, Massini Merzkani1, Haris Murad1, Yazen Al-Hosni1, Ronald Parsons3, Jason Wellen1, Su-Hsin Chang1, Tarek Alhamad1.
1Washington University School of Medicine at St.Louis, St Louis, MO, United States; 2Saint Louis University, Saint Louis, MO, United States; 3Emory University, Atlanta, GA, United States
Objective: Simultaneous pancreas-kidney transplantation (SPK) is a well-established treatment option for patients with diabetes mellitus and end-stage kidney disease, but SPK carries a 7-22% rate of technical failure. The impact of early pancreas graft function on subsequent kidney graft and patient survival in type 1 diabetic recipients of SPK is not well-defined.
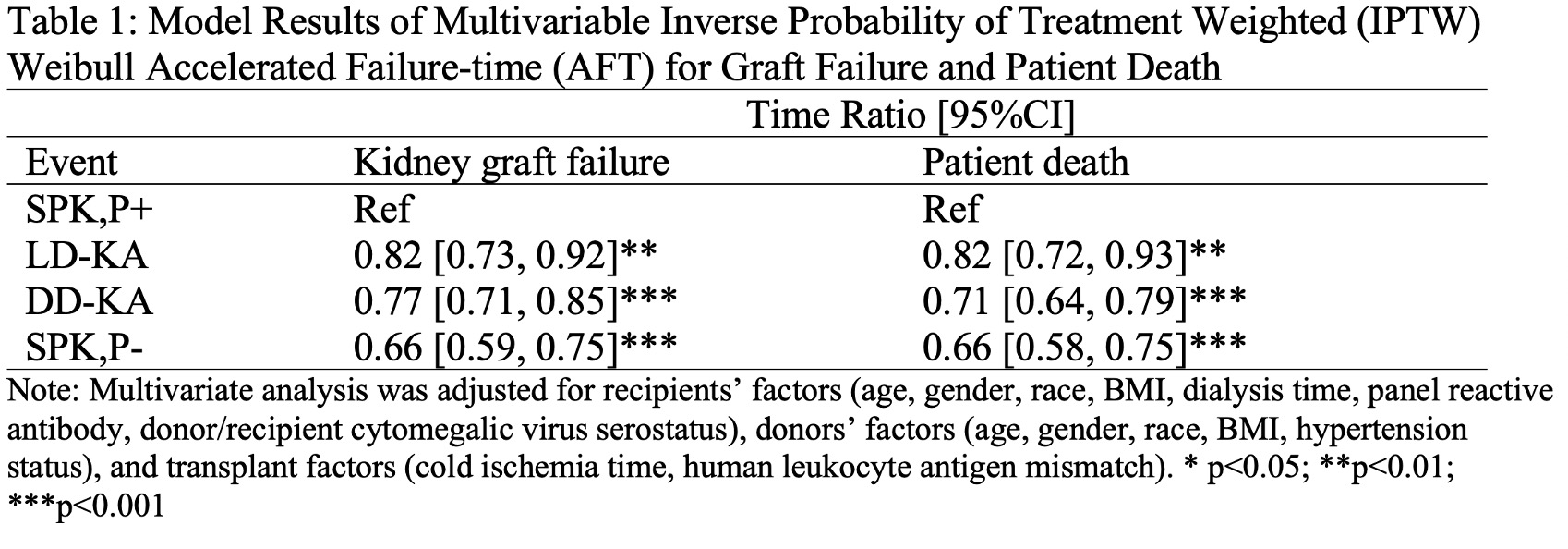
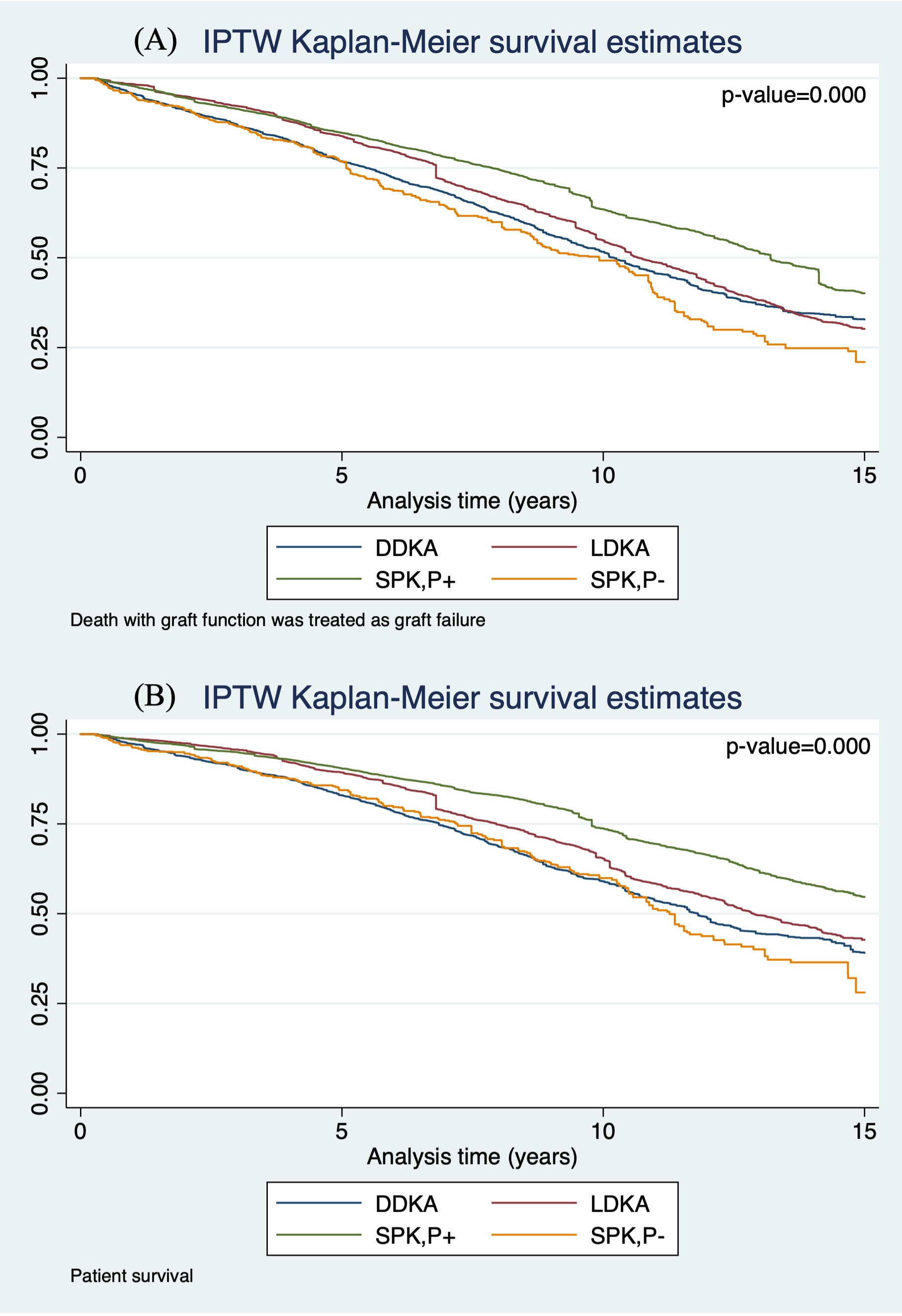
Methods: We examined national U.S. transplant registry data for type 1 diabetic patients who received SPK between 2000 and 2021 and survived the first 3 months with a functioning kidney. Transplant patients were categorized as: deceased‐donor kidney transplant alone (DDKA), living‐donor kidney transplant alone (LDKA), SPK recipients with a functioning pancreas graft 3 months posttransplant (SPK,P+), or SPK recipients with pancreas graft failure within 3 months posttransplant (SPK,P-). Associations of transplant type with kidney graft failure and patient survival through September 2021 were estimated by multivariable inverse probability of treatment weighted (IPTW) accelerated failure-time (AFT) models, with weights estimated using generalized boosted regression.
Results: Compared to SPK,P+ recipients, LDKA had 18% less graft survival time (TR: 0.730.820.92) and 18% less patient survival time (TR: 0.720.820.93), DDKA had 23% less graft survival time (TR: 0.710.770.85) and 29% less patient survival time (TR: 0.640.710.79), and SPK,P- had 34% less graft survival time (TR: 0.590.660.75) and 34% less patient survival time (TR: 0.580.660.75). Compared to LDKA, SPK,P- had 19% less graft survival time (TR: 0.700.810.94) and 19% less graft survival time (TR: 0.690.810.95). Compared to DDKA recipients, SPK,P- had 14% less graft survival time (TR: 0.760.860.97). No difference was found for patient survival time between SPK,P- and DDKA.
Conclusions: SPK recipients with functioning pancreas grafts within 3-month posttransplant have better kidney allograft and patient survival compared with LDKA and DDKA. Early pancreas graft failure results in inferior kidney and patient survival time compared to kidney transplant alone.
This study was supported by grant 4746 from the Foundation for Barnes-Jewish Hospital.

right-click to download
