Acute tubular injury and necrosis do not lead to meaningful elevations in donor-derived cell-free DNA (dd-cfDNA)
Sridhar Allam8, Peale Chuang4, Matthew Cooper3, Alexander Wiseman5, Thin Thin Maw6, Nikhil Agrawal1, Grigory Shekhtman1, Jijiao Zeng1, Dhiren Kumar7, Edmund Huang2.
1Kidney Transplant, CareDx, Brisbane, CA, United States; 2Medicine, Cedars Sinai Medical Center, Los Angeles, CA, United States; 3Surgery, Georgetown University School of Medicine, Washington DC, DC, United States; 4Medicine, Metrolina Nephrology, Charlotte, NC, United States; 5Medicine, CENTURA HEALTH-PORTER ADVENTIST HOSPITAL, Aurora, CO, United States; 6Medicine, University of Southern California, Los Angeles, CA, United States; 7Medicine, Virginia Commonwealth University, Richmond, VA, United States; 8Medicine, Medical City Transplant Institute, Fort Worth, TX, United States
KOAR registry.
Introduction: Associations between non-rejection histologic diagnoses and dd-cfDNA have not been extensively characterized. We explored these associations inkidney transplant recipients enrolled in the Kidney allograft Outcomes AlloSure Registry (KOAR, NCT03326076).
Methods: For-cause and surveillance biopsies with NR (no rejection or other abnormalities, except IF/TA) or acute tubular injury/necrosis (ATI/ATN), and paireddd-cfDNA within 30 days were included. The incidence of a composite outcome (eGFR decline > 25%, rejection, and de novo donor-specific antibody detection) at 12 months after biopsy was also assessed.
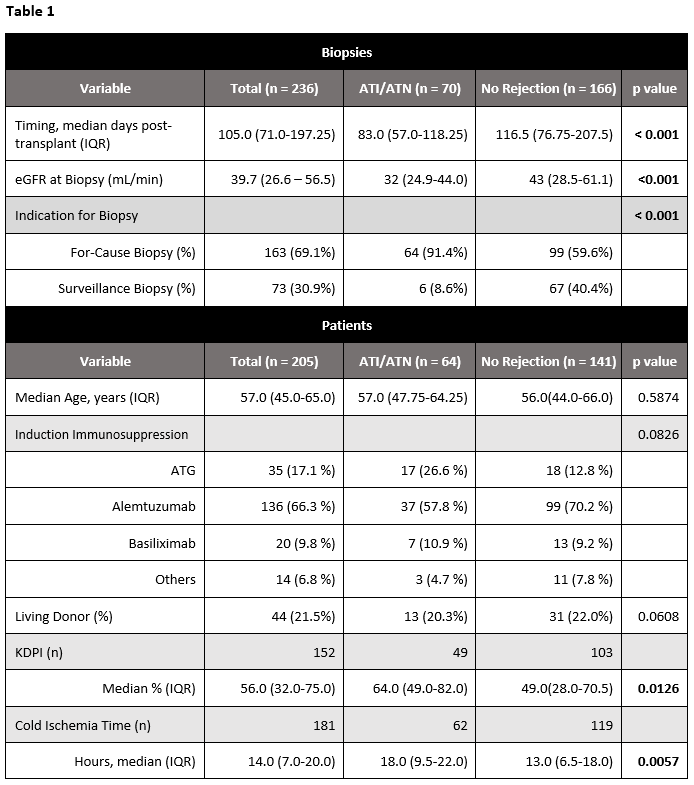
Results: 166 biopsies (141 patients) with NR and 70 biopsies (64 patients) with ATI/ATN were included; compared to patients with ATI/ATN, patients with NRhad lower KDPI (49% vs 64%, p <0.05) and shorter cold ischemia time (13 vs 18 hours, p<0.01). ATI/ATN biopsies were more likely to be for-cause (91.4% vs59.6%, p<0.001), earlier post-transplant (83.0 vs 116.5 days, p<0.001), and occur at lower eGFRs (43 vs 32 mL/min, p<0.001) (Table 1).
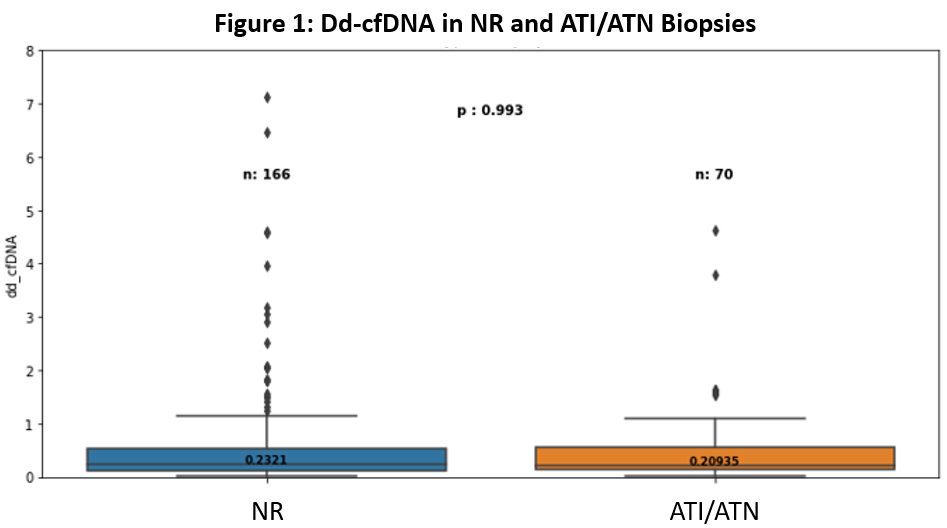
There was no significantdifference in median dd-cfDNA between NR (0.23%, IQR: 0.11 - 0.53) and ATI/ATN (0.21%, IQR: 0.13 - 0.55) biopsies (p = 0.993) (Figure 1). When patients werestratified by dd-cfDNA at the time of their first biopsy (< 0.5% vs ≥ 0.5%), there was a non-significant trend towards a higher incidence of the 12-month clinicalcomposite among those with dd-cfDNA ≥ 0.5% (27.5% vs 12.9%, p=0.53), with eGFR decline being most common (78.5% of events).
Conclusions: Our findings suggest that acute tubular injury/necrosis is not associated with substantial elevations in dd-cfDNA. The use of dd-cfDNA to identifypatients with non-actionable histologic findings (including ATI/ATN) may allow more nuanced clinical decision-making and reduce the number of unnecessarybiopsies.

right-click to download
