Pediatric liver transplantation: twenty-five-year experience at a single center
Dario N Teran1, Maria F Fernandez1, Leonardo Montes1, Dolores Garcia Hervas2, Diego A Ramisch1, Juan Rey3, Silvia Niveyro3, Pablo Barros Schelotto1, Julio Trentadue2, Carolina Rumbo4, Gabriel E Gondolesi1.
1Cirugía Hepatobiliar y Trasplante Multiorgánico, Hospital Universitario Fundación Favaloro, Caba, Argentina; 2Unidad de Internacion y Cuidados Intensivos Pediatricos, Hospital Universitario Fundación Favaloro, Caba, Argentina; 3Servicio de Anestesiologia, Hospital Universitario Fundación Favaloro, Caba, Argentina; 4Unidad de Hepatología y Trasplante Hepático Pediatrico, Hospital Universitario Fundación Favaloro, Caba, Argentina
Introduction: Pediatric liver transplantation (Tx) is a worldwide accepted therapy for those disorders that generate severe and irreversible acute and chronic liver diseases. We aim to report our 25-year experience, performing liver transplantation in children at a single center.
Material and methods: Retrospective analysis of patients <18 years old who underwent primary Tx or re-transplant (reTx) of the liver between January 1995 and December 2021 at a single center. Demographic data, time on the waiting list, indication and type of Tx, length of hospital stay, ischemia times, complications, overall graft and patient survivals were analyzed. Survival analysis was also performed comparing 2 different groups, G1: 1995-2008 and G2: 2009-2022. Statistical analysis was performed with SPSS version 25.0.
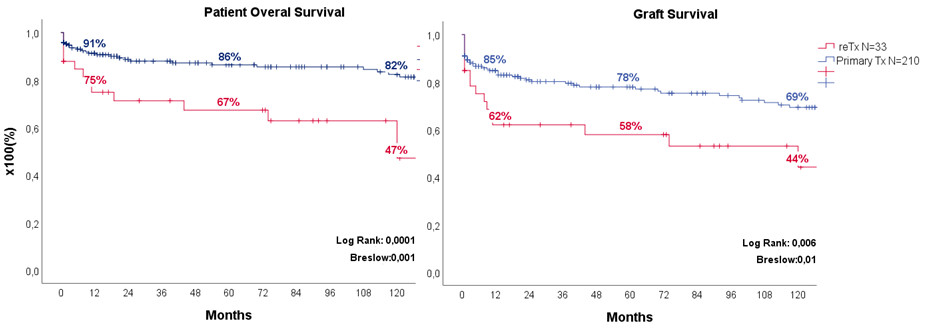
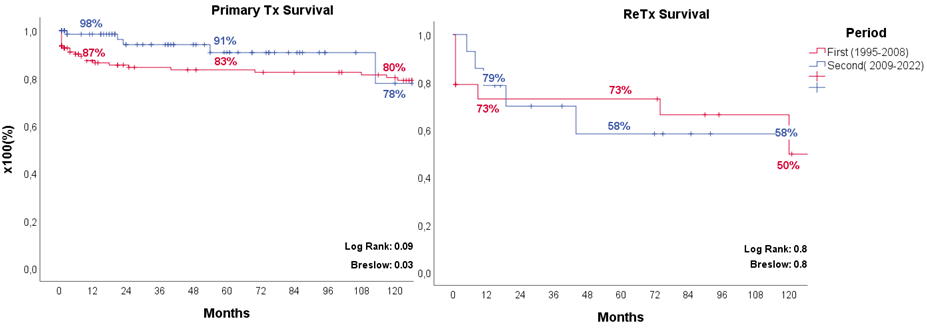
Results: A total of 243 Tx were done, 210 (86%) were primary Tx, 29 were re-Tx and 4 had a 3rd Tx, and 122 (50%) were female. The median age was 33 months (R=1-208), median weight was 13 kg (R=4-74 and z score weight for age -1.07 ± 1.5) and mean height of 100±35 cm (z score height for age -1,7 ± 1,8). Indications for Tx were: 88 (42%) biliary atresia, 33 (16%) cryptogenic acute liver failure, 24 (11%) fulminant viral hepatitis (HAV), 15 (7%) autoimmune hepatitis, 14 (7%) Alagille`s syndrome, 17% others. Re-Tx. were performed due to: chronic ductopenic rejection in 12 cases, arterial thrombosis in 7, primary graft dysfunction in 7, biliary complications in 4 and others in 3. The mean time on the waiting list for cadaveric Tx was 81 ± 191 days, mean post Tx hospitalization was 28±24 days (12±13 ICU and 15±19 general ward). One hundred fourteen (47%) Tx were performed with living donor; 129 (53%) with cadaveric grafts, of them 61(47%) with partial graft. The mean cold and warm ischemia time were 250±245 minutes and 44±42 minutes respectively: 402±127* and 45±17 minutes for cadaveric donors and 85±67* and 43±12 for living donors of cold and warm ischemia time (* p=0.001). The most frequent surgical complications were: 49 (20%) biliary (30 leaks and 19 strictures), 14(6%) hepatic artery thrombosis (11 early and 3 late), 10 (4%) portal vein (8 thrombosis and 2 stenosis), the remaining 10% were other complications (postoperative bleeding, acute ventral hernia, surgical wound infection, peritonitis); 14 (6%) cases of PTLD. Figure 1 shows patient and graft survival at 1, 5 and 10 years for those who received primary Tx and re-Tx. Figure 2 shows patient’s survival divided in primary Tx and re-Tx.
Conclusions: The most frequent cause of primary Tx is biliary atresia, while for re-Tx is chronic rejection. The most frequent early complication was bile leak, and the most frequent late complication was chronic rejection. Long-term survivals exceed the results from other regional and international centers.