Outcomes of liver transplantation at an argentinean program with 25 years of experience
Dario N Teran1, Maria F Fernandez1, Leonardo Montes1, Victoria Atencio2, Pablo A Farinelli1, Diego A Ramisch1, Guillermo Orce3, Francisco Klein4, Silvina Yantorno2, Pablo Barros Schelotto1, Valeria Descalzi2, Gabriel E Gondolesi1.
1Cirugía Hepatobiliar y Trasplante Multiorgánico , Hospital Universitario Fundación Favaloro, Caba, Argentina; 2Unidad de Hepatología y Trasplante Hepático, Hospital Universitario Fundación Favaloro, Caba, Argentina; 3Unidad de Anestesiología, Hospital Universitario Fundación Favaloro, Caba, Argentina; 4Unidad de Cuidados Intensivos, Hospital Universitario Fundación Favaloro, Caba, Argentina
Introduction: Liver transplant (LTx) is the treatment of choice for patients with end-stage liver disease. Twenty-five years after the program was started, several regulatory changes and reviewed guidelines, like the introduction of the MELD score, the prioritization criteria for HCC patients, and the effective treatment for HCV have impact transplant applicability and long term results. Different centers around the world have reported one year survivals close to 90% and 75% at 5 years. The aim of this study is to report long term outcomes of patients undergoing LTx at our center.
Material and methods: Retrospective analysis of patients >18 years old who received LTx or re-transplant (re-Tx) between June 1995 and March 2022. Donor’s and recipient’s clinical variables, including graft and patient were analyzed. Statistical analysis was performed with SPSS version 25.0.
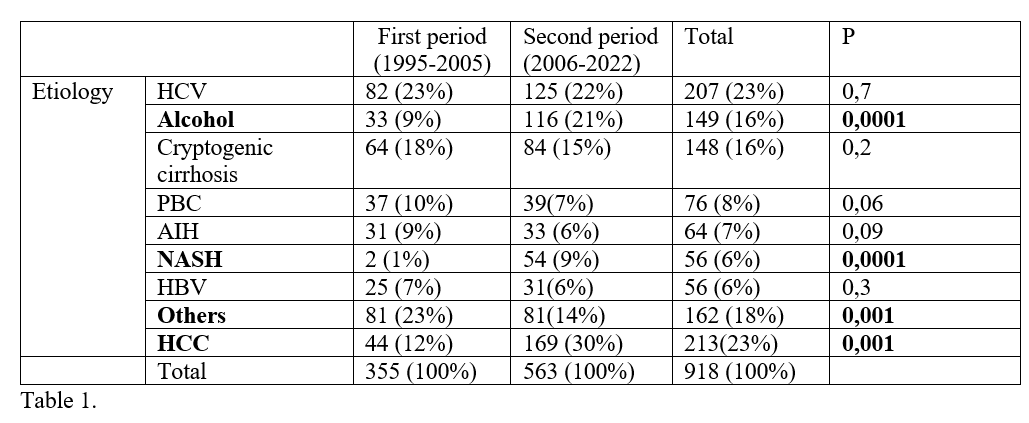
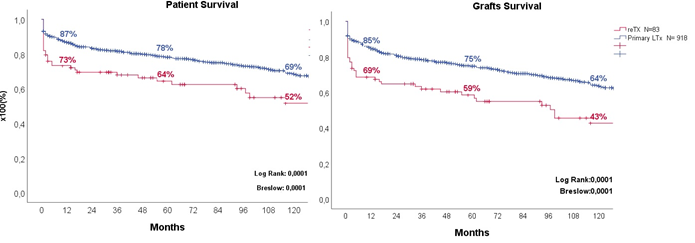
Results: A total 1246 LTx were performed during the period of study; 1001 (80%) were adults, 580 (58%) were male, mean age was 58 ± 13 years; 918 (92%) were primary transplants and 83 (8%) re--Tx. The indications for LTx were: 767(77%) Cirrhosis, 86 (9%) acute liver failure, 83(8%) re-Tx and 65 (6%) others. If we divide them by type of transplant: 933 (93%) were liver, 60 (6%) combined liver-kidney and others 1% (3 combined intestinal-liver, 2 liver-heart, 2 multivisceral and 1 liver-lung). Nine hundred and thirty-eight (93.7%) LTx were performed with cadaveric donor; 60 (6%) with living donor, 3 (0.3%) were part of domino liver transplant. Among the group of patients that received cadaveric grafts, 896 (95%) were whole liver and 42 partial grafts. Table 1 shows the main causes of primary LTx divided by periods. Eighty three cases (8%) were re-Tx: 21 due to ductopenic rejection (2%), 17 had arterial thrombosis (1.7%), 15 disease recurrence (1.5%), 9 ischemic cholangiopathy (1%), 6 PNF (0.6%), 3 (0.3%) graft dysfunction, others: 0.9%. Figure 1 show patient and graft survival at 1, 5 and 10 years for those who received primary LTx and reTx respectively.
Conclusion: Alcoholic liver disease, HCC and NASH had significantly increased in our second period of evaluation. According to current published international results, our center presents’ comparable results to other local, regional and international centers.