
The suppression of macrophage-mediated intestinal transplant rejection by C5a receptor antagonist
Chiyoshi Toyama1, Akira Maeda1, Shuhei Kogata1, Riho Yamamoto1, Takehisa Ueno1, Masafumi Kamiyama1, Yuko Tazuke1, Hiroshi Eguchi1, Katsuyoshi Matsunami3, Shuji Miyagawa2, Hiroomi Okuyama1.
1Department of Pediatric Surgery, Osaka Univesity, Suita, Japan; 2 International Institute for Bio-Resource Research, Meiji University, Kawasaki, Japan; 3Pharmaceutical Sciences, Hiroshima University, Hiroshima, Japan
Background: Complement component C5a promotes alloreactivity via C5a receptor 1 (C5aR1) on immune cells. However, the role of C5a in small intestinal transplantation immunity has not been reported. During an inflammatory response, macrophages are activated by C5a and produce various inflammatory cytokines. In the present study, we examined the effect of the C5aR1 antagonist PMX53 on macrophage function following small intestinal transplantation.
Methods: We established models by heterotopic intestinal transplantation using donor Dark Agouti and recipient Lewis rats. The rats were administered PMX53 starting on the day of operation until postoperative day 7. We assessed graft survival and performed HE staining of grafts and mixed lymphocyte reaction tests (MLR) using mixed cultures of T cells from lymph nodes and spleen cells from donors. Based on the complement activation results, we estimated serum levels of C5a and C5 mRNA levels in the graft on postoperative day 6. We also evaluated macrophage and T cell accumulation in the graft. To verify antibody-mediated rejection, we estimated anti-donor-specific antibodies in serum. Finally, we assessed the effect of PMX53 on macrophage differentiation and activation using bone marrow-derived macrophages (BMDMs).
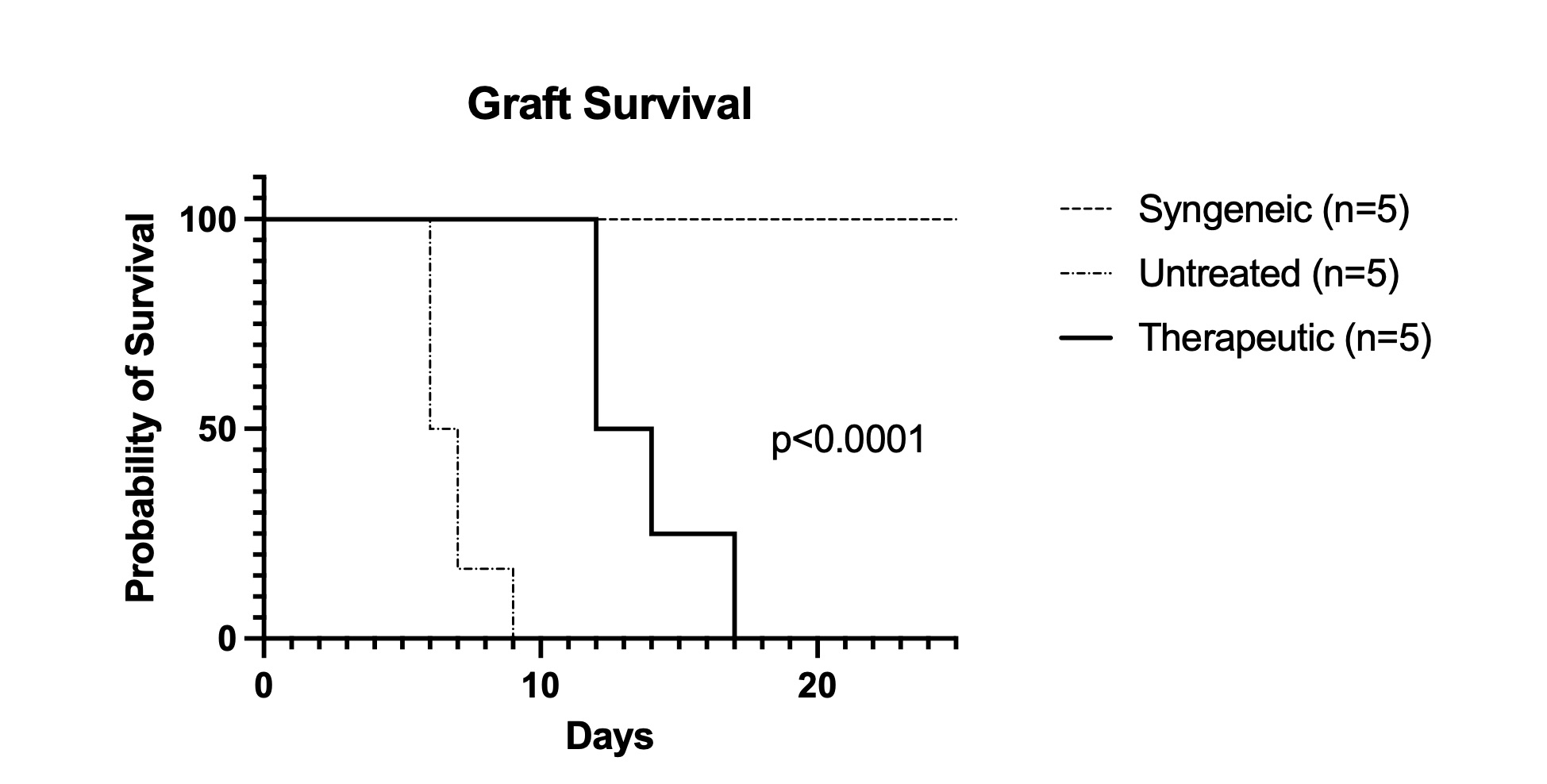
Results: Graft survival was significantly prolonged in the PMX53-treated group compared to that in the untreated group (6.6 vs 13.7 days, p<0.0001).
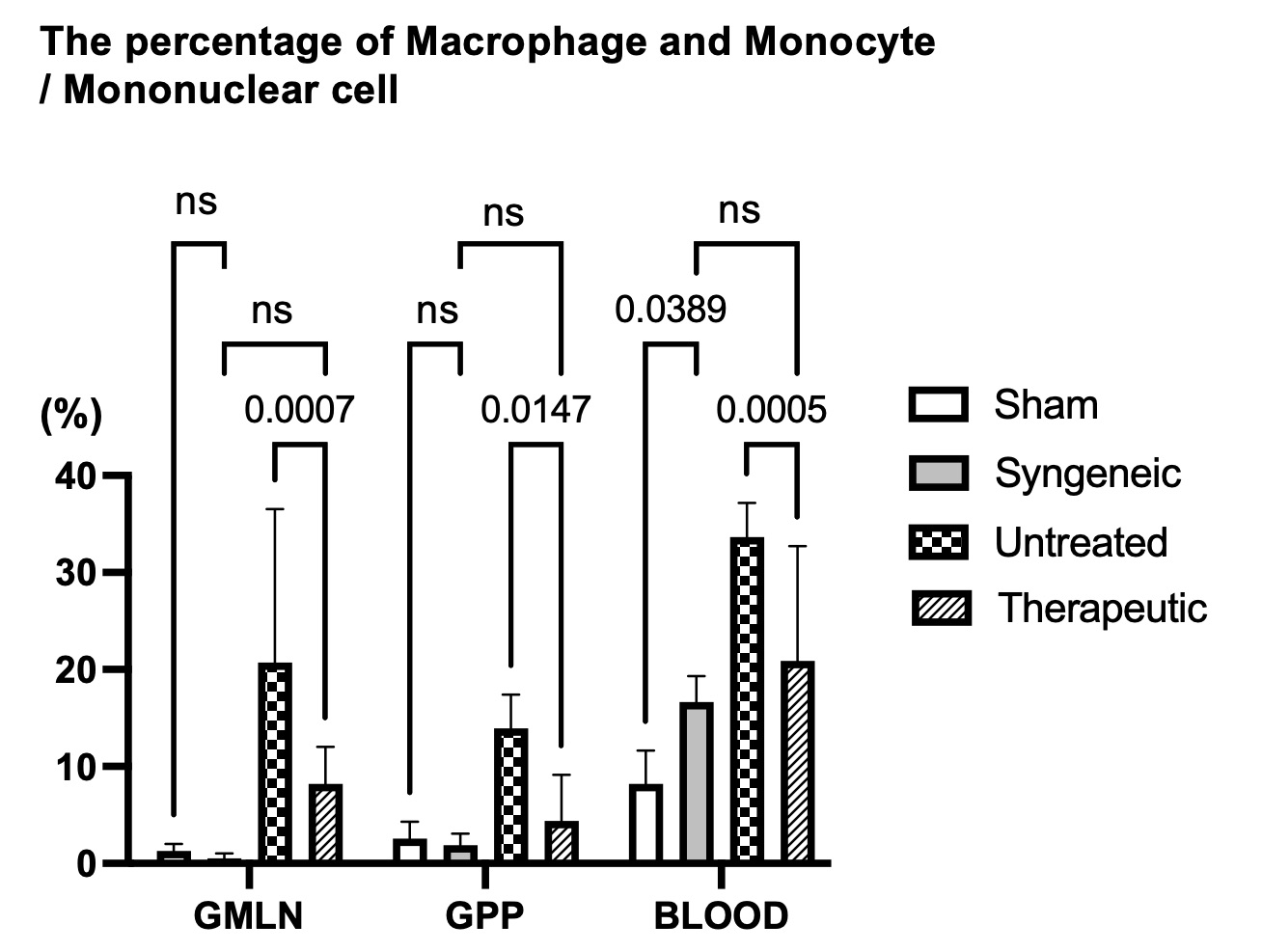
PMX53 treatment inhibited shortening of the graft villus, as shown by the histological evaluation, and significantly lowered the stimulation index of the MLR when compared to the untreated group (2.2 vs 5.1, p<0.0001). In the untreated group, serum C5a and C5 mRNA levels in the graft were elevated. In the treated group, macrophages accumulation in the mesenteric lymph nodes of graft and monocytes in blood were reduced when compared with the untreated group (17.7% vs 7.9%, p=0.0007; 34.3% vs 20.7%, p=0.0005).
Anti-donor-specific antibody levels in the treated and untreated groups were similar (MFI: 144.5 vs 116, p=0.068). PMX53 treatment decreased BMDM differentiation (CD11b/c+RT-1b+ cell: 56% vs 30%, p=0.001) as well as IL-1β and TNF-α mRNA expression levels in activated BMDMs (138 vs 45.8, p=0.0001 and 15.1 vs 4.22, p=0.0055).
Conclusion: A C5a receptor antagonist suppresses rejection after small intestinal transplantation. Inhibition of C5a/C5aR1 signaling appears to regulate macrophage differentiation and activation.

right-click to download
