Liver transplantation for metastatic neuroendocrine tumor in Argentina: outcomes from a multicenter study
Maria Florencia Fernandez1, Dario Teran1, Martin Fauda3, Lucas McCormack2, Valeria Descalzi1, Pablo Barros Schelotto1.
1Hospital Universitario Fundacion Favaloro, Caba, Argentina; 2Hospital Aleman, Caba, Argentina; 3Hospital Universitario Austral, Buenos Aires, Argentina
Introduction: Neuroendocrine tumors (NET) most common site of metastases is the liver and they usually present themselves as multiple, bilateral masses. For these patients, when the lesions are unresectable, the orthotopic liver transplantation (LT) presents a viable treatment option.
Patients and Method: Retrospective study of patients who underwent liver transplant due to NET metastases between 2007 and 2022 in 3 centers in Argentina. Patients were identified from existing databases at each unit, sent in an excel form and then put altogether in an IBM SPSS data sheet which was used to perform statistical analyses. Variables included were: age, sex, type of primary tumor, time of diagnosis of the liver metastases, type of graft, place of recurrence and patient survival.
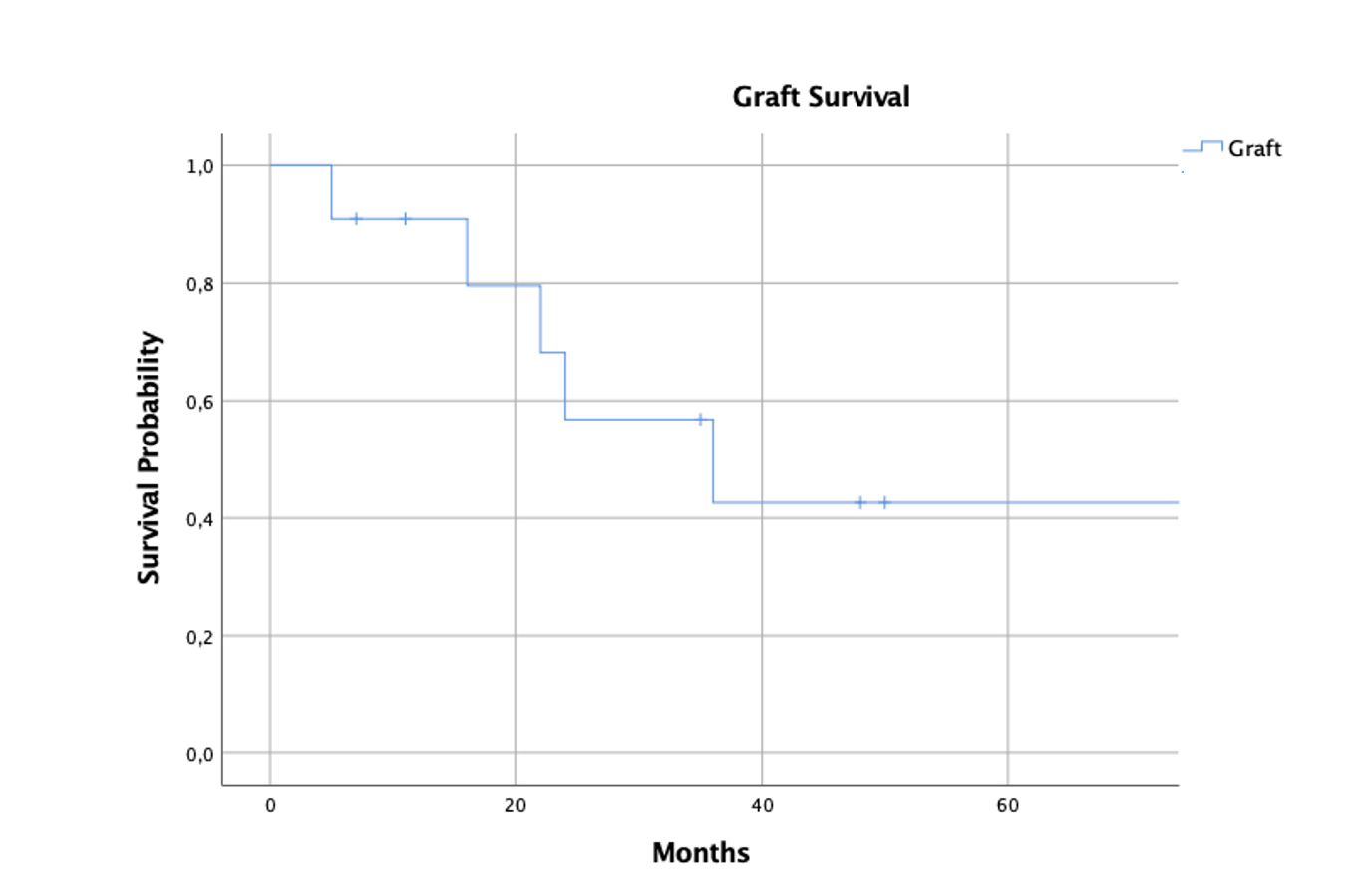
Results: Eleven patients received a LT due to irresectable liver NET metastases, 7 of them (64%) were women with a mean age of 49 ± 8 years old. In 8 patients (73%) the primary tumor was located in the small bowel and 10 cases (91%) were diagnosed with synchronous metastases. As part of the primary tumor resection, 4 enterectomies were performed (36%), 4 right hemicolectomies (36%) and 3 distal pancreatectomies with splenic preservation (8%). Afterwards, 8 patients (73%) were given somatostatin analogues and 1 everolimus. In 4 patients (36%), alternative treatments were employed to try to treat de liver metastases, including surgery, radiofrequency ablation and/or TACE. Seven patients (64%) were given additional MELD points and after a median of 3 months (range 1-17) 10 patients (91%) received a cadaveric liver (8 whole grafts and 2 splits). After the LT, patients continued receiving somatostatin analogues (n=8) and everolimus (n=1). As post-transplant complication, 2 patients presented graft rejection, 1 pseudoaneurysm of left hepatic artery and 1 ischemic cholangiopathy. Disease free survival was of 91%, 57% and 43% after 1-, 3- and 5-years post-LT (Fig. 1). Five patients had disease recurrence, 2 were treated with surgery, one with cisplatin and 1 underwent several medical treatments. Patient survival at 1, 3 and 5 years was of 91%, 78% and 78%, respectively (Fig. 2).
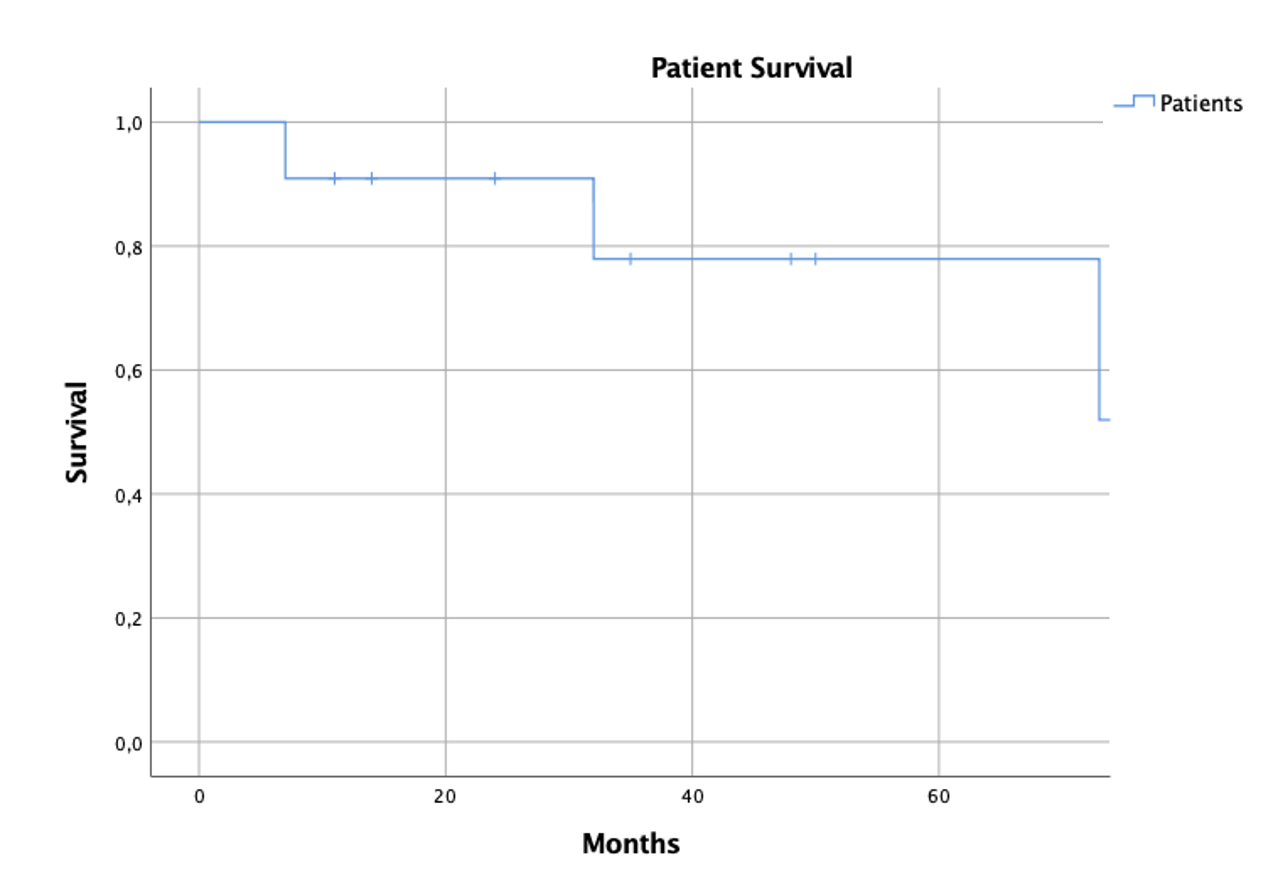
Discussion: Non-resectable NET liver metastasis confined to the liver is an accepted indication for liver transplantation. We have shown that patient’s survival is similar to the median survival of those who received a liver graft due to HCC being (in both cases) essential the correct selection of patients who will undergo the LT.

right-click to download
