Report of the first 70 pancreas transplant in a Latin-American center
Maria Florencia Fernandez1, Diego Ramisch1, Dario Teran1, Hugo Fraguas5, Rodolfo Marrugat3, Carla Musso4, Leonardo Montes1, Marcela Fortunato2, Pablo Raffaele2, Gabriel Gondolesi1.
1HPB and complex gastrointestinal surgery and abdominal organ transplant, Hospital Universitario Fundacion Favaloro, Caba, Argentina; 2Nephrology, Hospital Universitario Fundacion Favaloro, Caba, Argentina; 3Urology, Hospital Universitario Fundacion Favaloro, Caba, Argentina; 4Diabetology, Hospital Universitario Fundacion Favaloro, Caba, Argentina; 5Cardiovascular surgery, Hospital Universitario Fundacion Favaloro, Caba, Argentina
Introduction: In patients with diabetes mellitus (DBM) and end-stage renal disease (ESRD), kidney-pancreas transplantation has become an effective treatment option that reduces patient’s morbidity and increases survival compared with long-term dialysis treatment. Our aim is to show the experience in pancreas transplantation at a single center.
Method: Patients who received pancreas transplant (PT) from April 2008 to December 2021 were incorporated for analysis. Variables analyzed included: age, sex, comorbidities, type of diabetes, types of pancreas transplants, time in waiting list, preservation solution, time of cold and warm ischemia (CI and WI), hospital and ICU length stay, complications and overall patient’s and graft’s survival. All analyses were performed using IBM SPSS v25.0.
Results: A total of 70 PT were performed at our center: 67 (95%) simultaneous pancreas-kidney (PKT), 2 (3%) pancreas transplant alone (PTA) and 1 pancreas after kidney (PAK). Thirty-six were female (51%) with a mean age of 41 ± 9 years. Fifty-three patients (76%) had type 1 DBM and the mean BMI was 24 ± 3. The estimated time in waiting list was of 8 month (range 1-69); in 50 patients (71%) the preservation solution used was Wisconsin. All PT are performed with enteric drainage. The CI and WI time were of: 389 ±173 min and 37±16 min for kidney, and 487±104 min and 45±23 min for pancreas. The median ICU stay was of 7 days (range 2-67) and the total hospital stay of 18 days (range 6-121). Seventy-six kidney complications were reported in 46 patients (66%), 41 (54%) were due to urinary tract infection (UTI). Eight patients (11%) lost their kidney graft, being the most common reason cortico-resistant rejection (6, 75%). On the other hand, 64 pancreas complications were reported in 36 patients (51%), 20 of which were pancreatic fistula (31%) and 17 venous thrombosis. Fourteen patients (20%) suffered graft lost due to rejection (4, 29%) and duodenal perforation (4, 29%), 2 because of venous thrombosis (15 grafts were saved), 2 necrotizing pancreatitis 1 due to pancreatic fistula and 1 due to an hypovolemic shock. The overall pancreatic and kidney graft and patient’s survival are shown in Table 1.
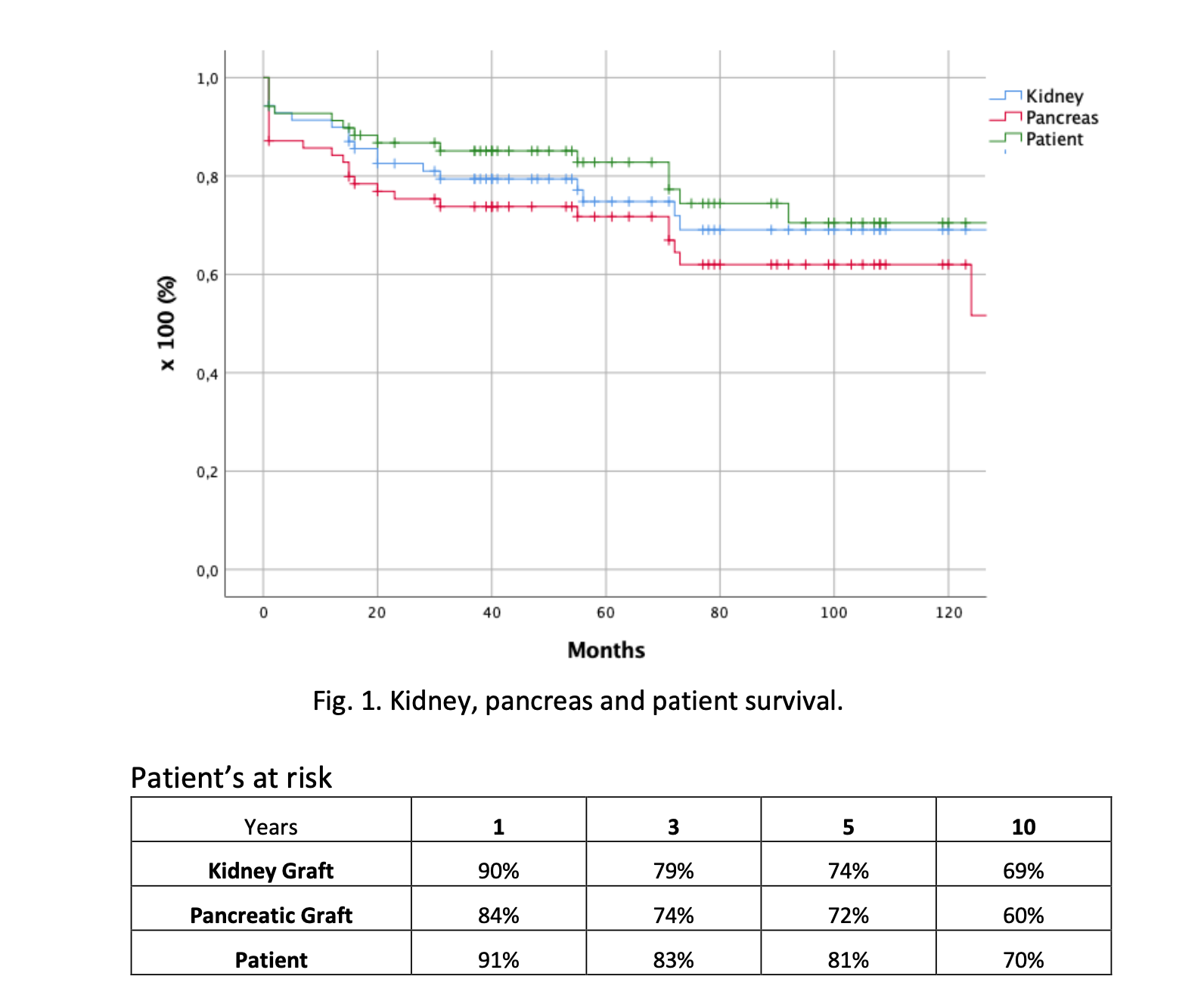
Discussion: Despite a careful selection of donors and recipients, an elevated number of pancreas and kidney complications occurred. Nevertheless, under a comprehensive team approach, most result minor, and acceptable graft and overall survival can be achieved.

right-click to download
