Diaphragmatic hernia following living donor hepatectomy: a systematic review of a rare and serious complication
Jayant Kumar1, Yaser Al-salmay1, Mauro Podda4, Isabella Reccia2,4, Francesco Virdis3, Piotr Witkowski1, John Lamattina1, Rolf Barth1, John Fung1, Diego di Sabato1, Ramesh Arasadnam1.
1The Transplantation Institute, University of Chicago Medical Centre, Chicago, IL, United States; 2General Surgery and Oncologic Unit, Policlinico ponte, San Pietro, Italy; 3Dipartimento DEA-EAS, Ospedale Niguarda Ca’ Granda, Milano, Italy; 4Department of Surgery, Calgiari University Hospital, Cagliari, Italy; 5Warwick Medical School, University of Warwick, Coventry, United Kingdom
Background: Living donor hepatectomy (LDH) is a complex and complicated surgical procedure with reported morbidity of 10 - 41 %. Although, the majority of these complications fall under Clavien Dindo grade I/II. Diaphragmatic hernia (DH) is one of the life-threatening and under-reported complications observed following LDH. The aim of this study is to determine the incidence of DH following LDH and identify implicating causative factors through a review of literature.
Methods: Following PROSPERO registration, a systematic database search was conducted for published literature between 2000 to 2022 on Jan 5th 2022. Seventeen studies with 37 cases were identified and included in this literature review (Fig 1).
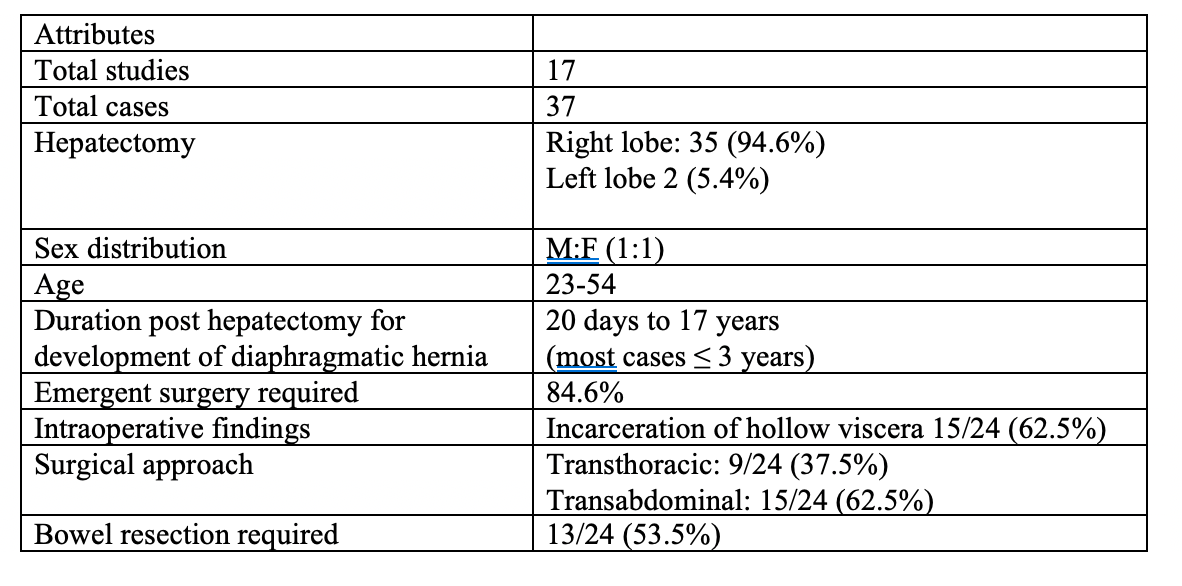
Results: Based upon the available data from the included studies and 7062 subjects who underwent LDH. Median patient age was 43 years (range 23-54) and most of the cases presented following right lobe hepatectomy 94.6% (35/37) within a period of <3 years. Incarceration of hollow viscera through diaphragmatic defect was presenting intraoperative feature in 62.5% donors, of which resection of bowel was required in 53.3% (Fig 2). Further, all patients had an uneventful postoperative recovery and were discharged in a satisfactory state with no reported recurrence in the literature.
Conclusions: The development of a DH following LDH should be considered a serious and life-threatening complication, which when recognized, requires immediate operative repair, as it is associated with a significantly higher risk of strangulation and incarceration of bowel segments.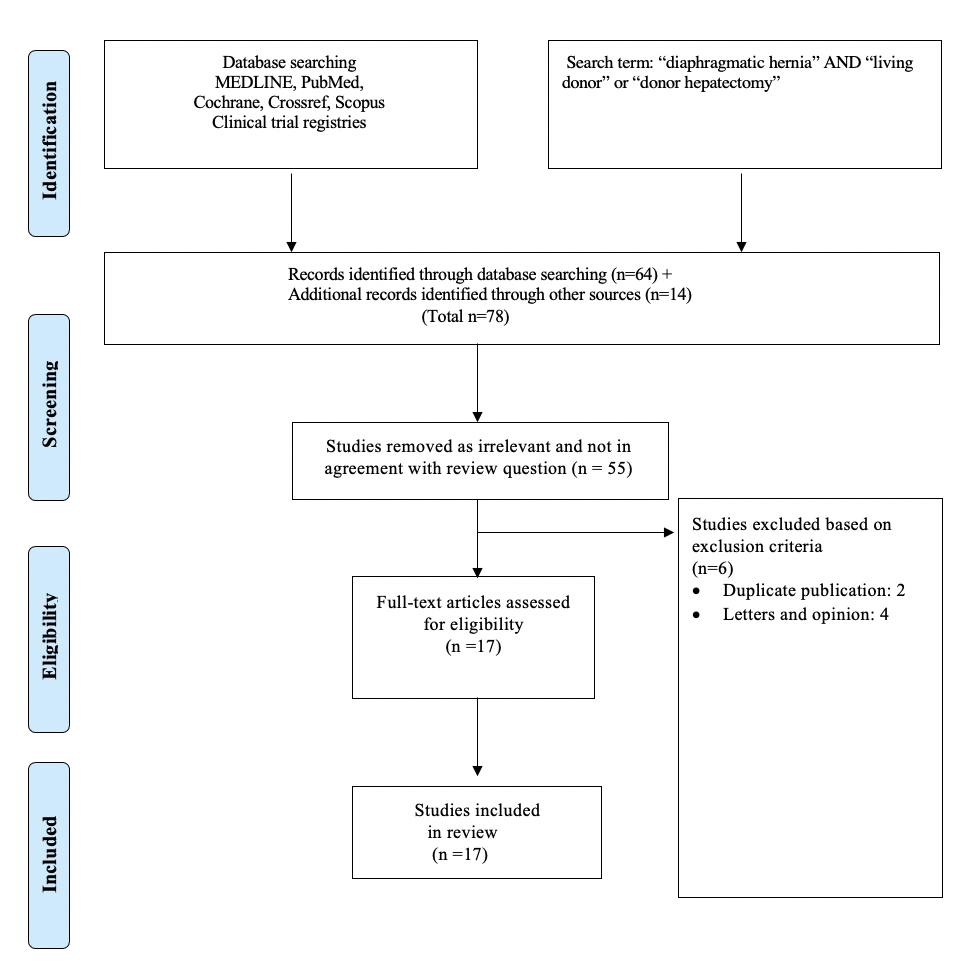

right-click to download
