
Outcomes with Omicron variant of severe acute respiratory syndrome 2 (SARS-CoV-2) virus in solid organ transplant recipients
Shweta Anjan1,2, Akshay Khatri1, Julia Bini Viotti1, Teresa Cheung1, Leopoldo A Cordova Garcia1, Jacques Simkins1,2, Matthias Loebe2,3, Anita Phancao2,4, Christopher B O’Brien2,5, Neeraj Sinha2,6, Gaetano Ciancio2,3, Rodrigo M Vianna2,3, David Andrews7, Lilian M Abbo1,2, Giselle Guerra2,8, Yoichiro Natori1,2.
1Department of Medicine, Division of Infectious Disease, University of Miami Miller School of Medicine, Miami, FL, United States; 2Miami Transplant Institute, Jackson Health System, Miami, FL, United States; 3Department of Surgery, University of Miami Miller School of Medicine, Miami, FL, United States; 4Department of Medicine, Division of Cardiology, University of Miami Miller School of Medicine, Miami, FL, United States; 5Department of Medicine, Division of Hepatology, University of Miami Miller School of Medicine, Miami, FL, United States; 6Department of Medicine, Division of Pulmonology, University of Miami Miller School of Medicine, Miami, FL, United States; 7Department of Pathology, University of Miami Miller School of Medicine, Miami, FL, United States; 8Department of Medicine, Division of Nephrology, University of Miami Miller School of Medicine, Miami, FL, United States
Introduction: Solid organ transplant (SOT) recipients are at high risk for severe disease with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. Emerging variants of concern have disproportionately affected this population. Data on severity and outcomes with the Omicron variant in SOT recipients is limited.
Methods: Single-center, retrospective cohort study of SOT recipients diagnosed with SARS-CoV-2 infection from December 18, 2021, to January 18, 2022, when prevalence of the Omicron variant was more than 95% in the community. Univariate and multivariate logistic regression analysis was performed to identify risk factors for hospital admission.
Results: We identified 166 SOT patients – 125 (75.3%) kidney, 27 (16.2%) liver, 10 (6.0%) lung, 8 (4.8%) heart, 9 (5.4%) combined transplants [Table 1]. SARS-CoV-2 vaccine series was completed in 59 (35.5%) recipients.
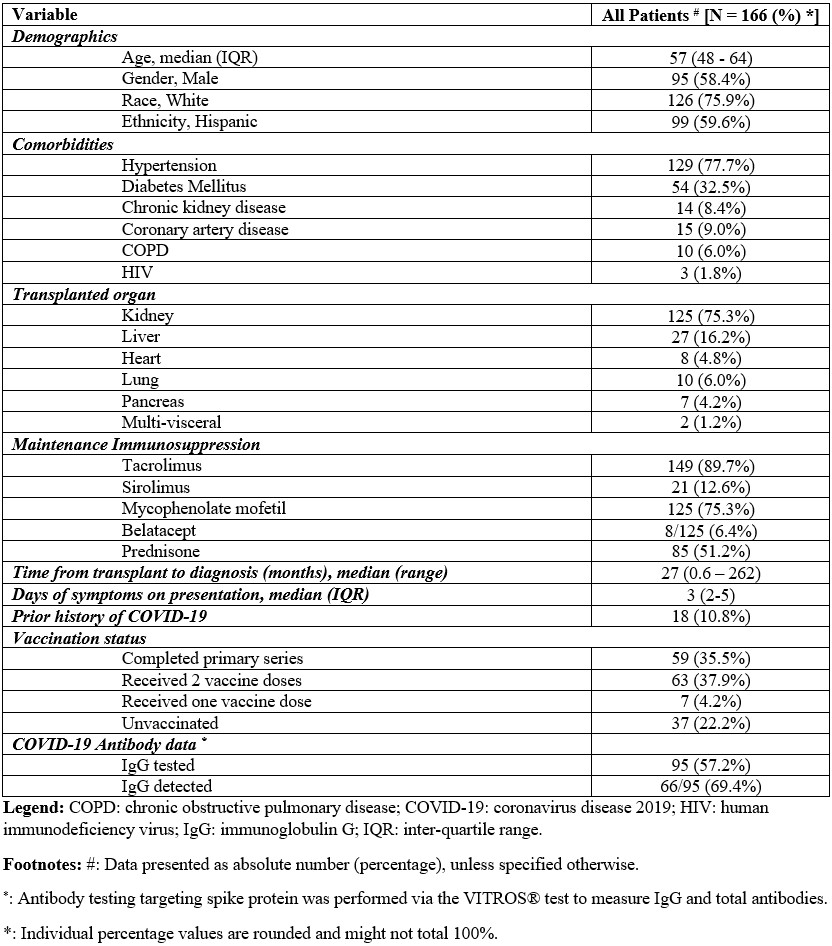
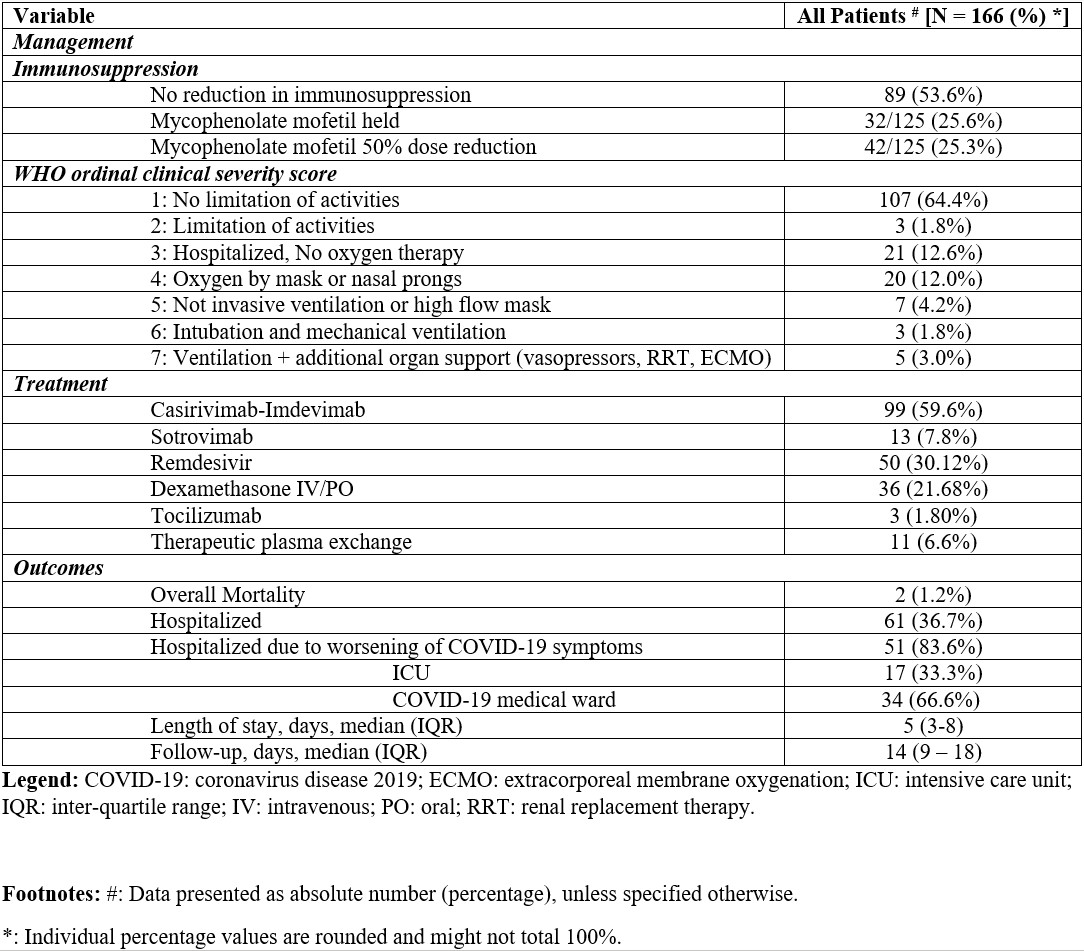
Ninety-nine (59.6%) and 13 (7.8%) recipients received casirivimab/imdevimab and sotrovimab, respectively [Table 2]. Fifty-one (83.6%) recipients required hospital admission, of which 17 (33.3%) required intensive care unit level of care. Anti-metabolite agents were decreased or stopped in 74/125 (59.2%) patients. Median time of follow up was 14 days (IQR, 9-18), with mortality reported in 2 (1.2%) patients. Kidney function was compared among patients before, at time of, and 1-month post-diagnosis of COVID-19. Median creatinine was 1.3mg/dL (range 0.5–9.4), 1.3mg/dL (range 0.6–10.7) and 1.27mg/dL (range 0.6–10.4) respectively. Creatinine was statistically significantly increased after COVID-19 diagnosis (p<0.001), however 1-month post-transplant, there was no statistical difference when compared to prior to transplant (p=0.31). Risk factors identified for hospital admission were African American race (p<0.001, Odds ratio [OR] 4.00, 95% Confidence Interval [CI] 1.84–8.70), history of coronary artery disease (p=0.031, OR 3.50, 95% CI 1.12–10.87), and maintenance immunosuppression with corticosteroids (p=0.048, OR 2.00, 95% CI 1.01–4.00).
Conclusion: Similar to the general population, we found low mortality and high hospital admission rate in SOT recipients with omicron variant infection. Further studies to investigate the efficacy of newer treatments are necessary, even as outcomes continue to improve.
