Controlling the cytokine stom with therapeutic plasma exchange: the MTI experience with solid organ transplant recipients
Adela Mattiazzi1,3, Shweta Anjan2,3, Juliano Riella3,4, Raphaella Ferreira3, Luke Preczewski3, Jacques Simkins2,3, Yoichiro Natori2,3, Giselle Guerra1,3.
1Medicine/Nephology, University of Miami, Miami, FL, United States; 2Medicine/ Infectious Disease, University of Miami, Miami, FL, United States; 3Transplant, Miami Transplant Institute. UM/JMH, Miami, FL, United States; 4Surgery/Transplant, University of Miami, Miami, FL, United States
Introduction: The solid organ transplant recipient (SOTr) have suffered a tremendous impact from coronavirus pandemic. The use of immunosuppressants and frequent associated medical comorbidities put this population at extreme risk for developing SARS-CoV-2 associated pneumonia. SARS-CoV-2-related mortality is higher in SOTr. It has been hypothesized that cytokine release storm (CRS) is the leading cause of ARDS in COVID-19 and timely control of this inflammatory response may improve outcomes. We report our experience of using therapeutic plasma exchange (TPE) to improve outcomes by tackling CRS in a timely manner.
Methods: This is a single-center, retrospective cohort study of SOTr diagnosed with SARS-CoV-2 infection from April 2020 to April 2021. All the patients received severity stratified institutional protocolized treatment and TPE was initiated based on clinical and inflammatory parameters of CRS and ARDS. TPE patients received Methylprednisolone 250 mg x 3 days then 125 mg x 2 days, followed by Prednisone 60 mg x 2 days and then 30 mg x 2 days. All patients received prophylaxis with omeprazole, ivermectin 0.2 mg/Kg daily for 2 days followed by 2 additional doses 2 weeks later, and trimethoprim/sulfamethoxazole (renally adjusted) 3 times weekly for 3 months. Laboratory markers, immunosuppression, WHO severity score pre- and post-TPE therapy and outcomes including mortality were analyzed. For risk factor analysis for mortality, we performed logistic regression analysis for univariate analysis. After that, based on the univariate analysis, we developed multivariate model. We conducted multiple logistic regression analysis with stepwise backward elimination.
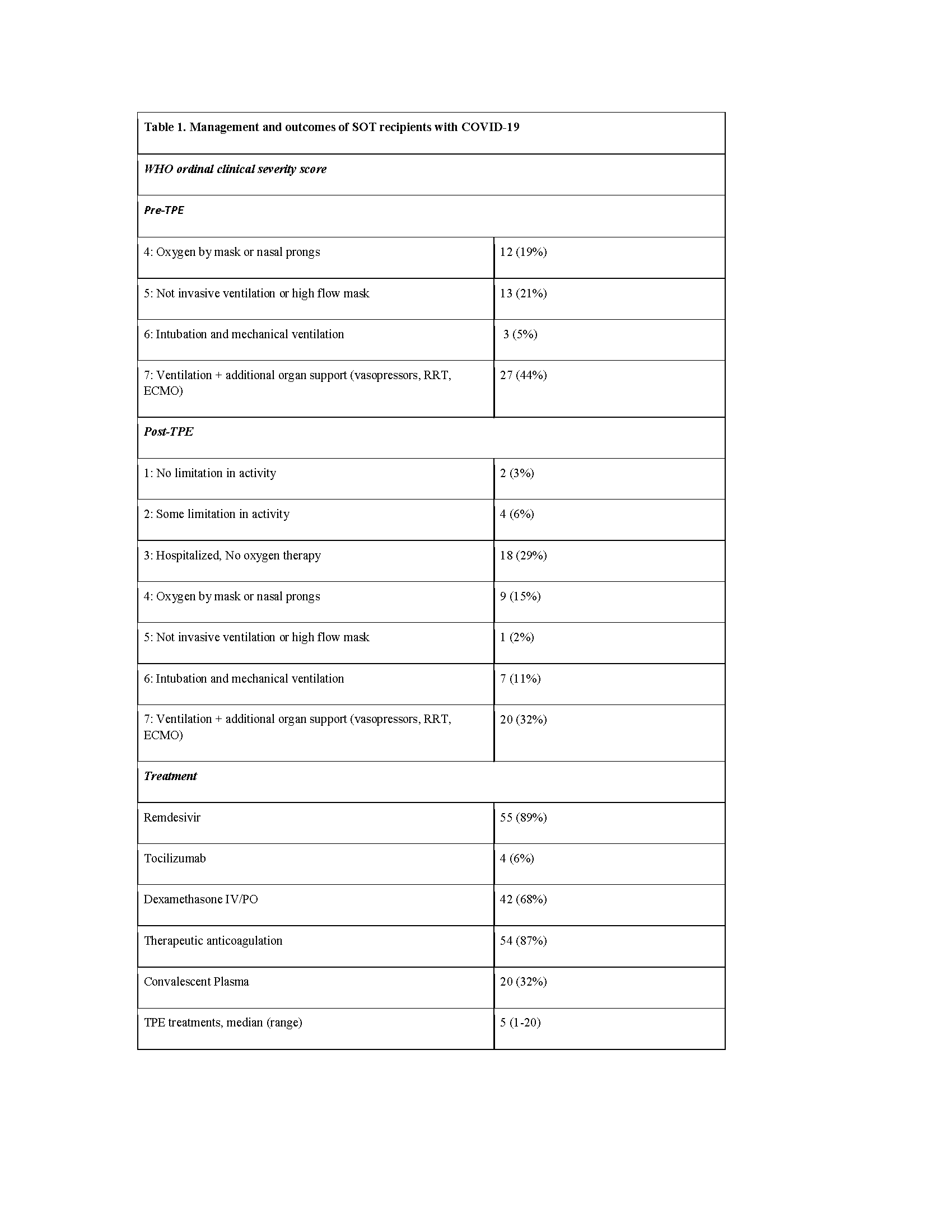
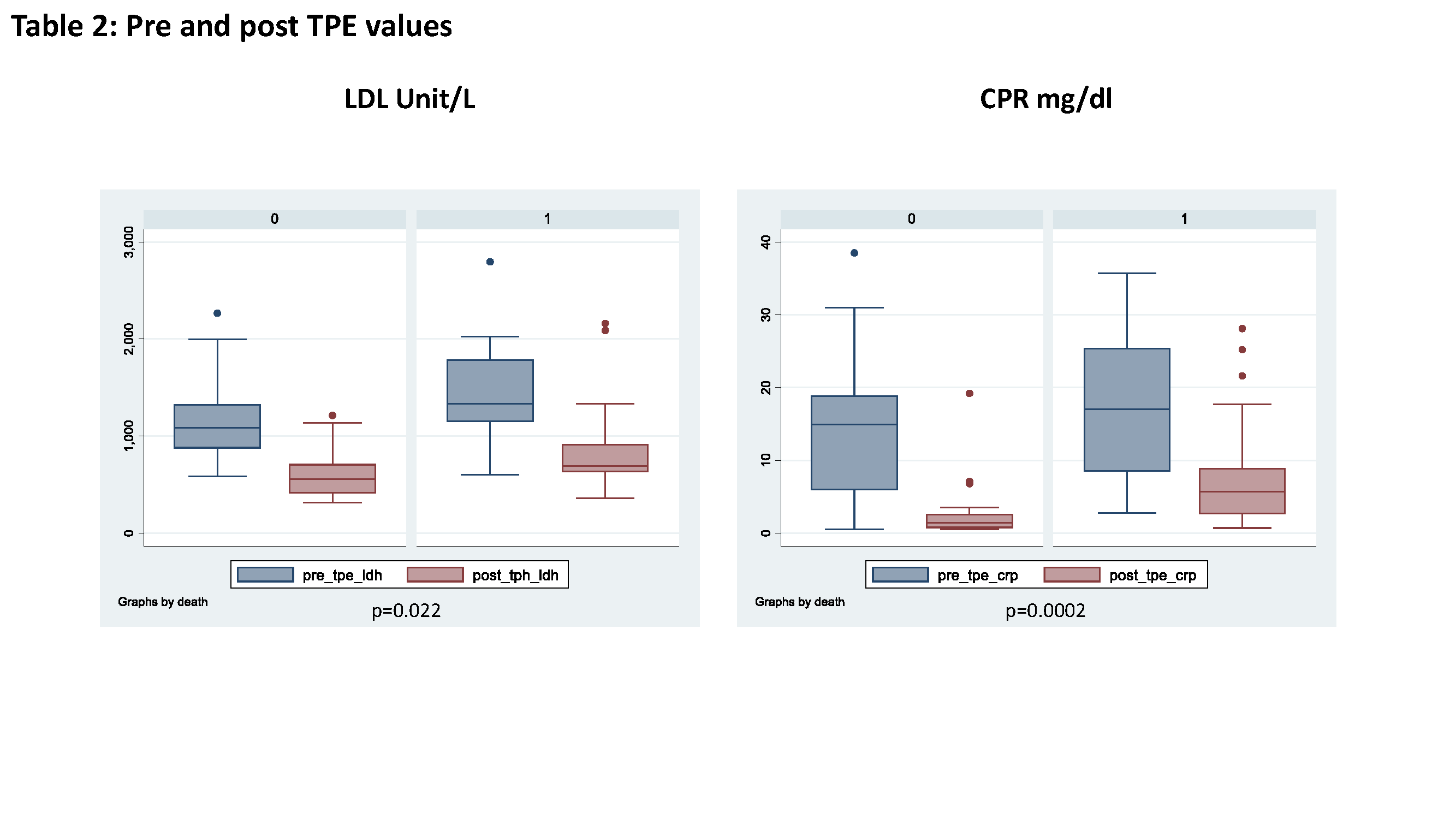
Results: 62 patients were followed for median of 141 days (range 8-376). The median age was 60 years (range 28-78), 65% were male, 76% had hypertension, 55% had diabetes and 81% were overweight with a BMI > 25 kg/m2. 90% were of Hispanics and Afro-Caribbean ethnicity. The most common transplanted organ was kidney with 54 patients (87%), followed by liver with 4 patients (6.5%). Time from transplant to diagnosis was 10 months(median, IQR 4-37) and time from symptoms to admission was 3 days (median, IQR 2-5). 79% of the patients were admitted to an intensive care unit (ICU). Tacrolimus (77%) and mycophenolate mofetil (87%) were the most common immunosuppressant drugs used with mycophenolate mofetil being held in 75% of the patients. The median of TPE sessions was 5 (range 1-20). Prior to TPE, there were 27 patients (44%) requiring ventilatory support and additional support (vasopressors, Renal Replacement Therapy (RRT) or Extracorporeal Membrane Oxygenation (ECMO)). A reduction of 32% support on the 27 patients was observed after TPE. The WHO severity score pre- and post-TPE therapy was statistically significant (p<0.001). The overall mortality was 26/62 patients (42%). Secondary infections were diagnosed in 35/62 (56%) of patients with 77 % leading to mortality and of those, 38 % were fungal infections. The median length of stay was 42 days (range 2-207). 4/54 (7%) kidney transplant recipients developed graft failure at 9, 18, 139 and 344 days respectively; and 4/54 (7%) had episodes of acute rejections at 1,14, 22 and 124 days of COVID diagnosis, respectively. Univariable analysis showed that older age and elevated LDH pre TPE and the lack of decline on LDH, D Dimer, CRP and ferritin values post TPE were risk factors for mortality ( p=0.001; 0.022; 0.006; 0.004; 0.0002 and 0.043, respectively). The presence of a secondary infection was correlated with increased likelihood of death from 25% to 55% and it occurred with a mean of 8 days (range 1-65) from its diagnosis. Multivariate analysis showed older age and CRP values post TPE as risk factors for mortality (p=0.015 and 0.04, respectively).
Conclusion: SARS-CoV-2 infection with cytokine storm leading to ARDS leads to high mortality, especially in the SOTr. TPE appears to be a valuable tool to control the cytokine storm by reducing the systemic inflammatory response and improving the overall critical state. Alongside with older age, we observed that high levels of LDH pre TPE and the persistent high levels of the other inflammatory parameters, specifically CRP post TPE and secondary infections, were predictors of mortality. Further research is needed to establish if these findings can lead to clinical guidelines.