A prediction model for antibody response to three vaccines against SARS-CoV-2 among solid organ transplant recipients
Jennifer Alejo1, Teresa PY Chiang1, Jonathan Mitchell1, Jake D Kim1, Aura T Abedon1, Robin K Avery2, Aaron AR Tobian3, Jacqueline M Garonzik-Wang5, Daniel S Warren1, Dorry L Segev4, William A Werbel2, Sunjae Bae1.
1Surgery, Johns Hopkins, Baltimore, MD, United States; 2Medicine, Johns Hopkins, Baltimore, MD, United States; 3Pathology, Johns Hopkins, Baltimore, MD, United States; 4Surgery, NYU Langone Health, New York, MD, United States; 5Surgery, University of Wisconsin, Madison, WI, United States
Johns Hopkins COVID-19 Vaccine Study Team.
Background: Solid organ transplant recipients (SOTRs) show impaired immune response to SARS-CoV-2 vaccines. A prediction model for immune response to SARS-CoV-2 vaccines could enable targeted antibody monitoring and vaccine dose adjustments in SOTRs during potential epidemic/endemic circulations of SARS-CoV-2.
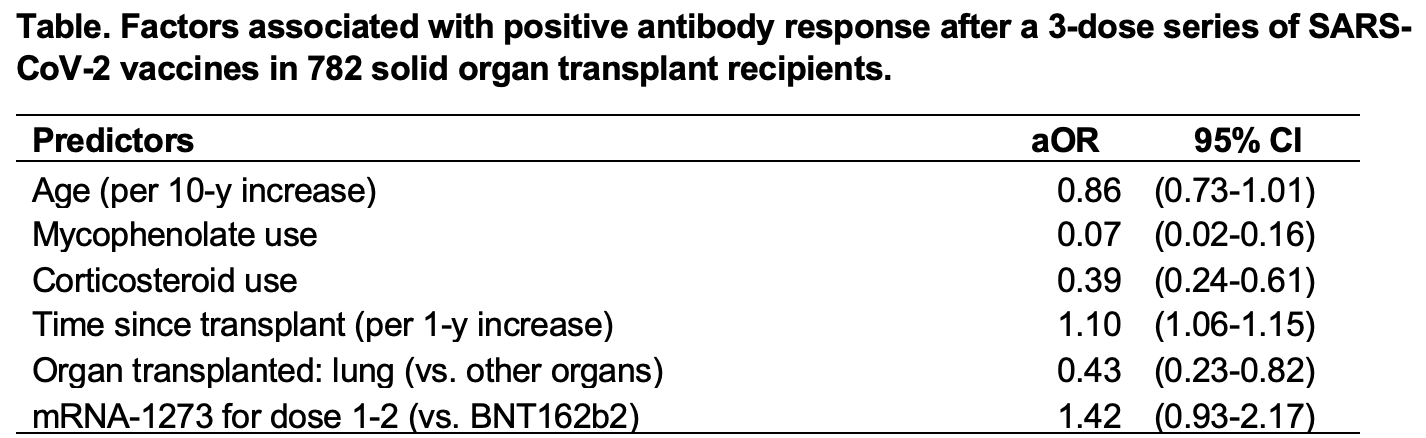
Methods: We studied 782 SOTRs recruited from across the United States who received a 3-dose series of SARS-CoV-2 vaccines and underwent serologic testing for SARS-CoV-2 antibodies between 2-5 weeks after the third dose. We used gradient boosting and logistic regression to create prediction models for positive antibody response based on demographic, transplant-related, and immunosuppression-related clinical factors.
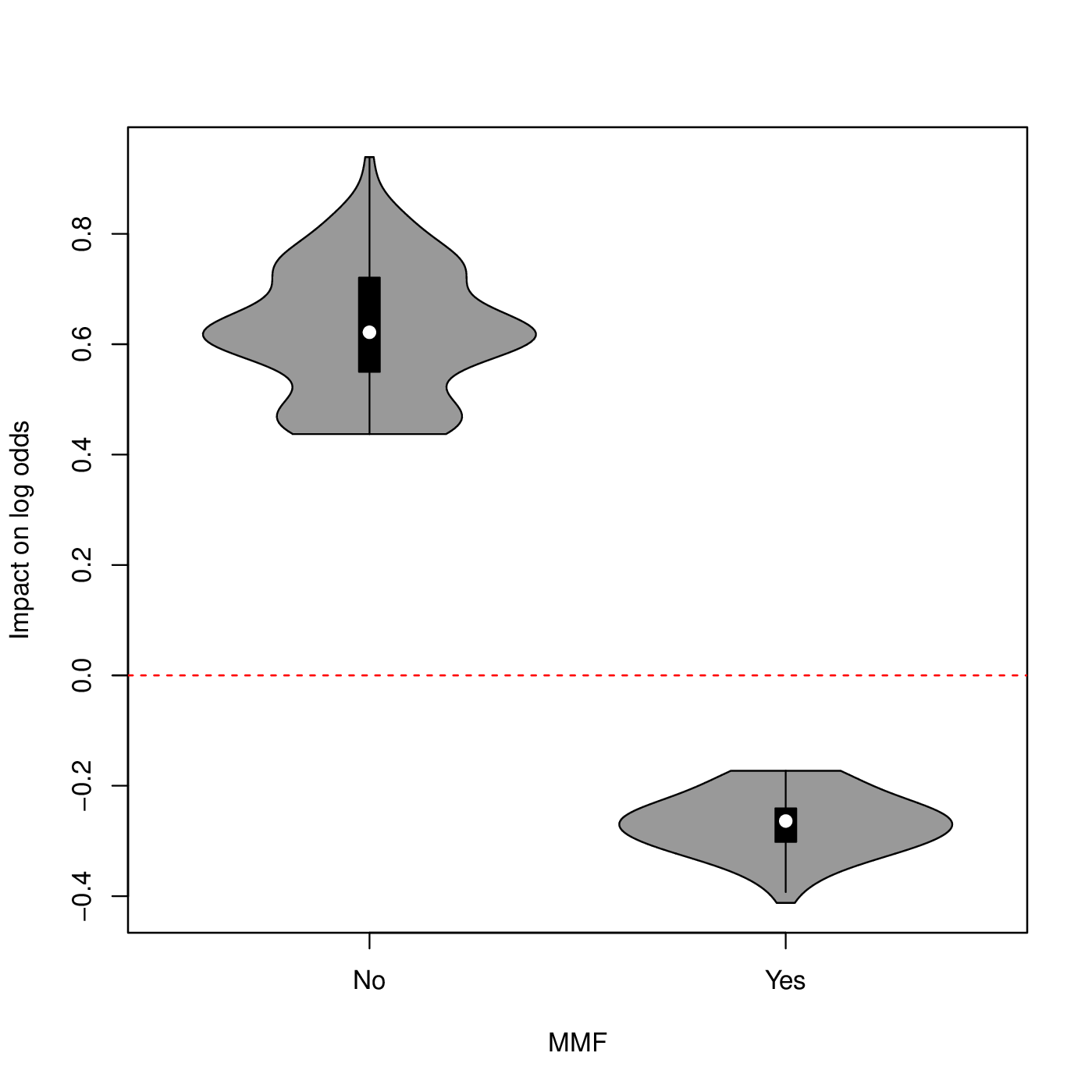
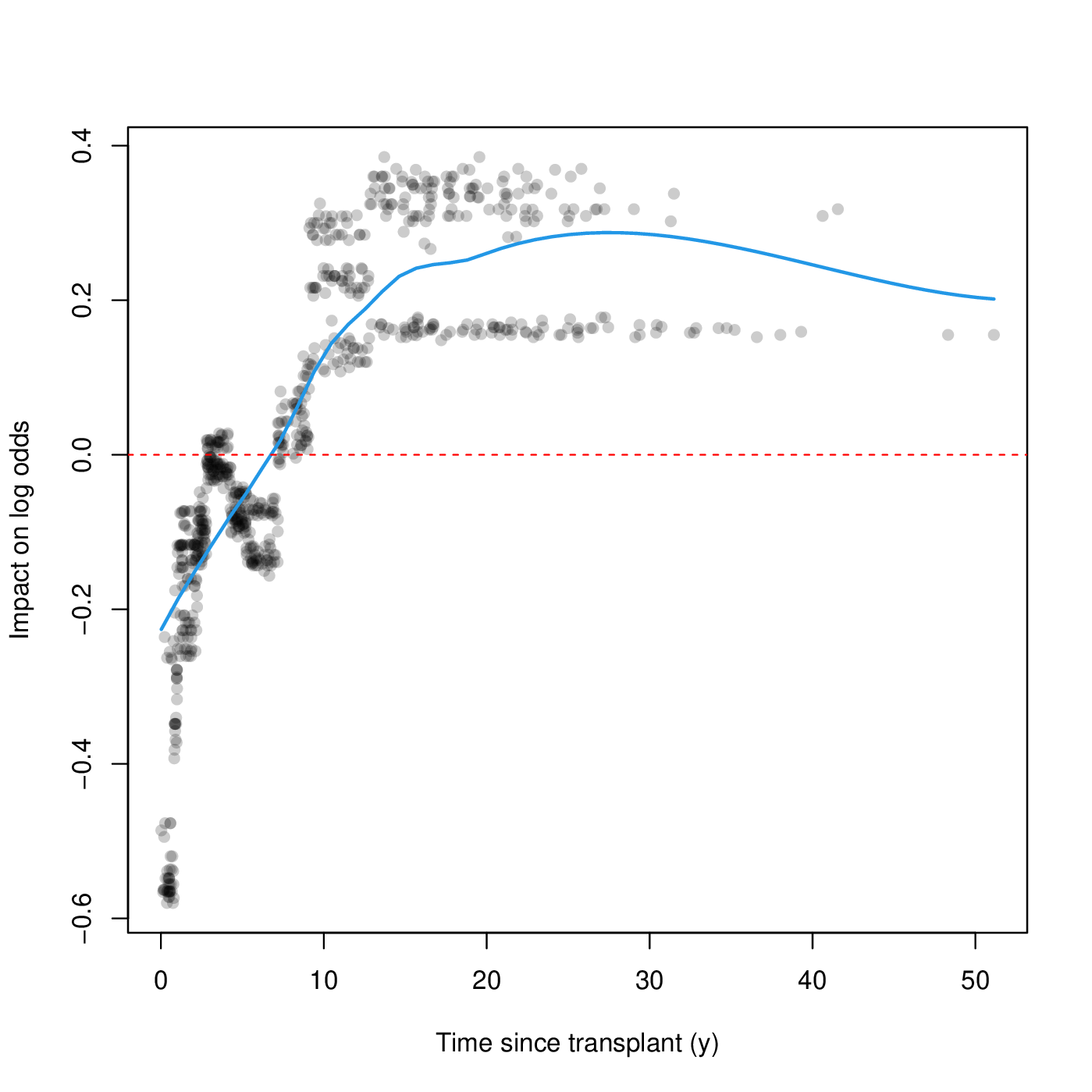
Results: Overall, 643 (82.3%) SOTRs had positive antibody responses. The gradient boosting model predicted positive antibody response with moderate accuracy (C-statistic, 0.790). The influential predictors of positive antibody response were mycophenolate avoidance (variable importance, 43.0%), longer time since transplant (31.2%), and corticosteroid avoidance (11.9%). The logistic model showed similar prediction accuracy (C-statistic, 0.790). Mycophenolate use (aOR, 0.07 [95% CI, 0.02-0.16]), corticosteroid use (aOR, 0.39 [95% CI, 0.24-0.61]), and time since transplant (per year; aOR, 1.10 [95% CI, 1.06-1.15]) showed significant association with positive antibody response.
Conclusion: Antibody response to a 3-dose SARS-CoV-2 vaccine series could be predicted with moderate accuracy in SOTRs. This prediction model could identify SOTRs with higher risks that warrant additional vaccine doses and antibody monitoring.
This work was supported by the Ben-Dov family; grants T32DK007713 (Dr. Alejo), The ASTS Fryer Resident Scientist Award (Dr. Mitchell), K01DK101677 (Dr. Massie), and K23DK115908 (Dr. Garonzik-Wang) from the National Institute of Diabetes and Digestive and Kidney Diseases; grant K24AI144954 (Dr. Segev) and K23AI157893 (Werbel) from the National Institute of Allergy and Infectious Diseases.
