
Deceased kidney donor acceptance criteria: a survey of Canadian transplant nephrologists, surgeons and urologists
Amanda Vinson1, Rahul Mainra2, Heloise Cardinal3, Christina Parsons4, Darin Treleaven5, Kyle Maru6, John Gill7.
1Medicine, Dalhousie University, Halifax, NS, Canada; 2Medicine, University of Saskatchewan, Saskatoon, SK, Canada; 3Medicine, Centre de recherche du Centre hospitalier de l’Université de Montréal, Montreal, QC, Canada; 4Medicine, Organ and Tissue Donation and Transplantation, Canadian Blood Services, Ottawa, ON, Canada; 5Medicine, McMaster University, Hamilton, ON, Canada; 6Canadian Blood Services, Toronto, ON, Canada; 7Medicine, The University of British Columbia, Vancouver, BC, Canada
Introduction: Kidney transplantation provides a quality of life and survival advantage for patients with end-stage kidney disease (ESKD) relative to remaining on dialysis. However, the number of patients on the transplant waitlist is steadily increasing relative to the number of available kidney donors. Despite this, while Canadian organ discard rates are not available, the proportion of discarded kidneys in the United States has paradoxically increased over time. While there is an abundance of literature regarding predictors of organ decline in the United States, to date, there are no data regarding the rate or rationale for deceased donor decline in Canada.
Methods: We performed an online survey (July 22-Oct 4, 2021) to assess deceased donor acceptance practices of Canadian transplant nephrologists, surgeons and urologists. Surveys were distributed by email to members of the Canadian Transplant Society. Surveys consisted of 3 sections of increasing donor complexity and respondents were asked whether they would accept or decline a hypothetical donor presented in the question stem, assuming there was a suitable recipient. The proportion of respondents completing the survey was determined, as were overall and donor scenario-specific acceptance rates amongst those providing responses.
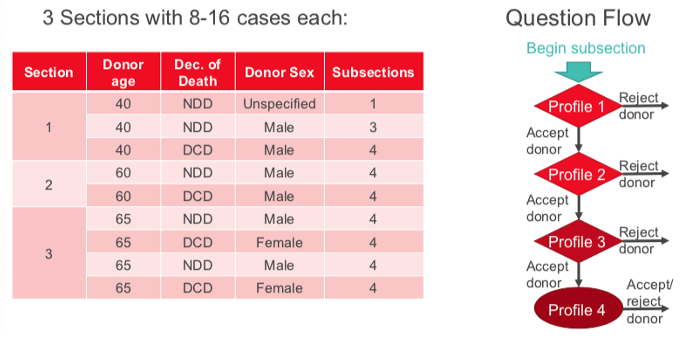
Results: A total of 81 respondents accessed the survey from 19 centers and seven provinces across Canada (all provinces with at least one transplant center). A total of 72 respondents (88.9%) answered at least one question and 16 respondents (22.2%) did not complete the survey. Donor acceptance rates for Sections 1 and 2 are demonstrated in Figure 2.
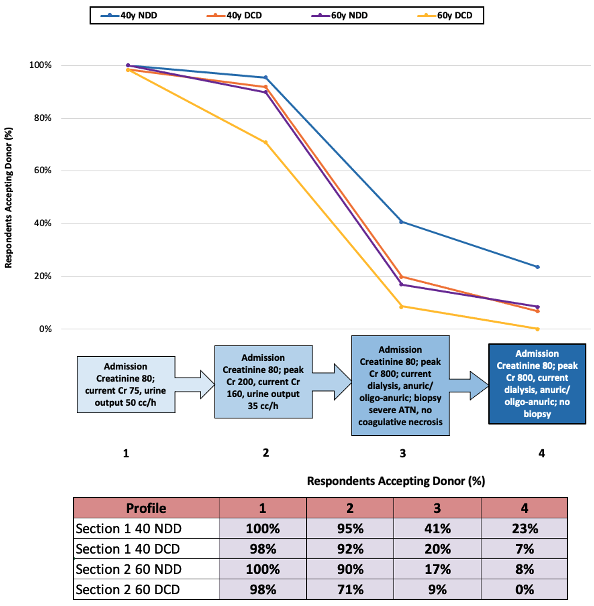
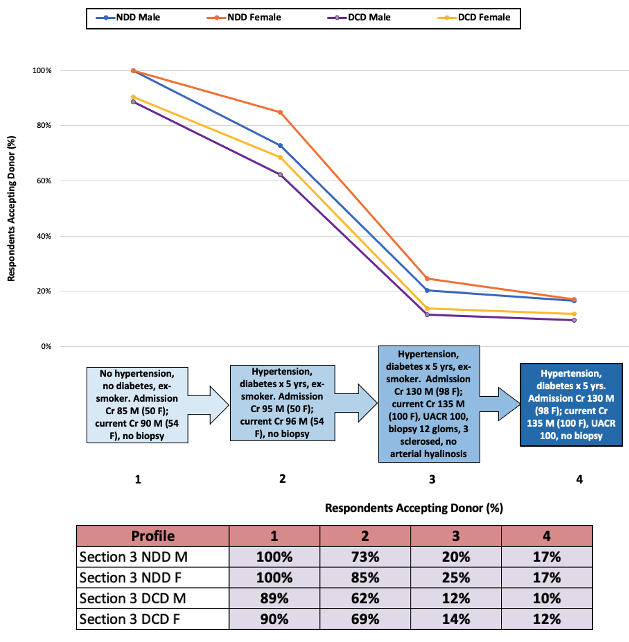
Overall acceptance rates were highest for the younger (40 years) donor scenarios and when the donor was NDD vs. DCD. The most pronounced drop in acceptance rates for all donor scenarios was between a non-dialysis dependent donor with recovering AKI (92% acceptance) and a donor with AKI requiring dialysis and a biopsy demonstrating ATN but no coagulative necrosis (20% acceptance). Acceptance rates for Section 3 are demonstrated in Figure 3. The most pronounced drop in acceptance rates for all donor scenarios was between a deceased donor with comorbidities but no CKD (85% acceptance) and a donor with CKD and a biopsy demonstrating 3 out of 12 glomeruli sclerosed, but no arterial hyalinosis (25% acceptance). Overall, advanced donor age, DCD donor status, AKI, CKD and comorbidity burden were all associated with an increased risk of deceased donor non-acceptance.
Conclusions: Given relatively high rates of donor decline and apparent heterogeneity in acceptance decisions, Canadian transplant specialists may benefit from additional education regarding the benefits achieved from even medically complex or “marginal” kidney donors for appropriate candidates relative to remaining on dialysis on the transplant waitlist.
