Trends of antibiotic resistance in E. coli, Klebsiella spp., Pseudomonas aeruginosa and Enterococcus spp. Urinary tract infection in renal transplant recipients from Pakistan over a decade
Sunil Dodani1, Asma Nasim1, Tahir Aziz2.
1Infectious Diseases, Sindh Institute of Urology and Transplantation, Karachi, Pakistan; 2Transplant Nephrology, Sindh Institute of Urology and Transplantation, Karachi, Pakistan
Introduction: Antimicrobial resistance is a major public threat worldwide. There has been an emergence of multi-drug resistant (MDR) bacterial infections over the last decade. MDR Klebsiella species have become one of the most common nosocomial pathogens in hospitals. In Pakistan, many studies reported a rising trend of resistance to antimicrobials in clinical isolates of Klebsiella species (spp.), E-coli, Pseudomonas aeruginosa and Enterococcus spp. Solid-organ transplant (SOT) recipients are more prone to infections, particularly with MDR organisms due to immunocompromised status, multiple hospital visits, and increased exposure to antibiotics. There is a paucity of data on antibiotic susceptibility patterns among renal transplant recipients from Pakistan. This study is conducted to find the trends in antimicrobial resistance patterns among common organisms isolated in the urinary tract over a 10-year period in renal transplant recipients. The aim is to guide the physicians regarding decisions over empirical antimicrobial choices.
Methods: Sindh Institute of Urology and Transplantation (SIUT) is a 700-bedded tertiary care hospital in Karachi, Pakistan. It has had a comprehensive renal transplantation program with more than 6500 transplantations now. A retrospective computerized data review of urine cultures from renal transplant recipients in 2010 and 2020 was conducted. The trend of E.coli, Klebsiella species (spp.) Pseudomonas aeruginosa and Enterococcus spp. were collected. The resistance pattern of amoxicillin-clavulanic acid, ceftriaxone (ceftazidime for Pseudomonas aeurginosa), piperacillin-tazobactam, ciprofloxacin, amikacin, co-trimoxazole, and imipenem were compared over the 10 years period.
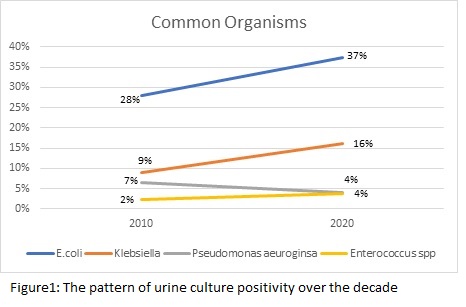
Results: A total of 2,088 out of 6,249 (33%) and 2902 out of 8,115 (36%) urine cultures were positive in 2010 and 2020 respectively. The most common organisms isolated and their trend in the last decade is shown in figure 1.
Over the decade, E-coli strains become 100% resistant to ciprofloxacin, ceftriaxone resistance has increased to 80%, and imipenem to 11%. In Klebsiella spp. imipenem resistance has increased to 19%. There is no significant change in the resistance pattern among Pseudomonas aeurginosa. Regarding Enterococcus spp. there is a rise in vancomycin resistance over the decade from 13% to 17% (Figure 2).
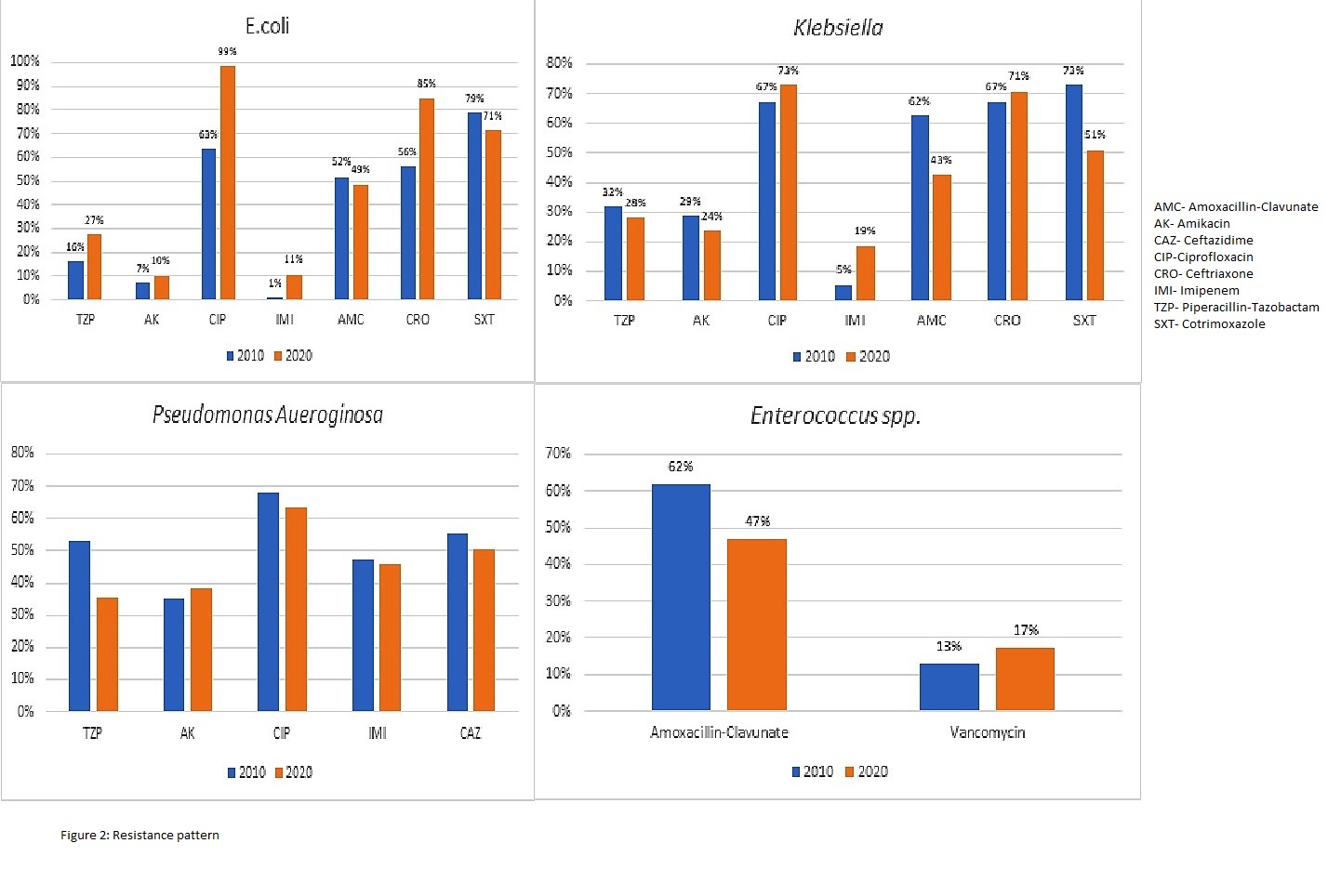
Conclusion: Resistance to broad-spectrum antimicrobials has been increased with a>10% increase in carbapenems resistance over the last 10 years. E-coli has particularly become more resistant over the decade. We are also seeing more vancomycin-resistant enterococcus. The alarming increase in resistance may lead to increased morbidity in renal transplant recipients because we are left with only injectable options. We need a robust stewardship program for judicious use of antimicrobials and better infection control measures to contain increasing resistance.
