One year survival comparison of deceased donor versus living donor hepatic pediatric transplantation. Meta-analysis
Alexandru Baetu1,3, Alexandrina Damașcan1, Andreea Moga2,3, Laura Bălănescu2,3, Radu Bălănescu2,3.
1Anesthesia and Intensive Care, Emergency Clinical Hospital for Children "Grigore Alexandrescu" Bucharest, Bucharest, Romania; 2Pediatric Surgery, Emergency Clinical Hospital for Children "Grigore Alexandrescu" Bucharest, Bucharest, Romania; 3University of Medicine and Pharmacy "Carol Davila" Bucharest, Bucharest, Romania
Introduction: The constant improvement of surgical techniques, immunotherapy and intensive care has significantly contributed to the rescue of children with extremely low chances of survival due to terminal liver disease. Probably the most important milestone in this advance was taking a transplant from a living donor. Studies published in recent years show a higher survival rate compared to grafts taken from brain-dead patients.
Purpose: This meta-analysis will attempt to highlight the one-year absolute survival of patients who received a transplant from a living donor(LDLT) compared to those who received a transplant from a brain-dead patient(DDLT).
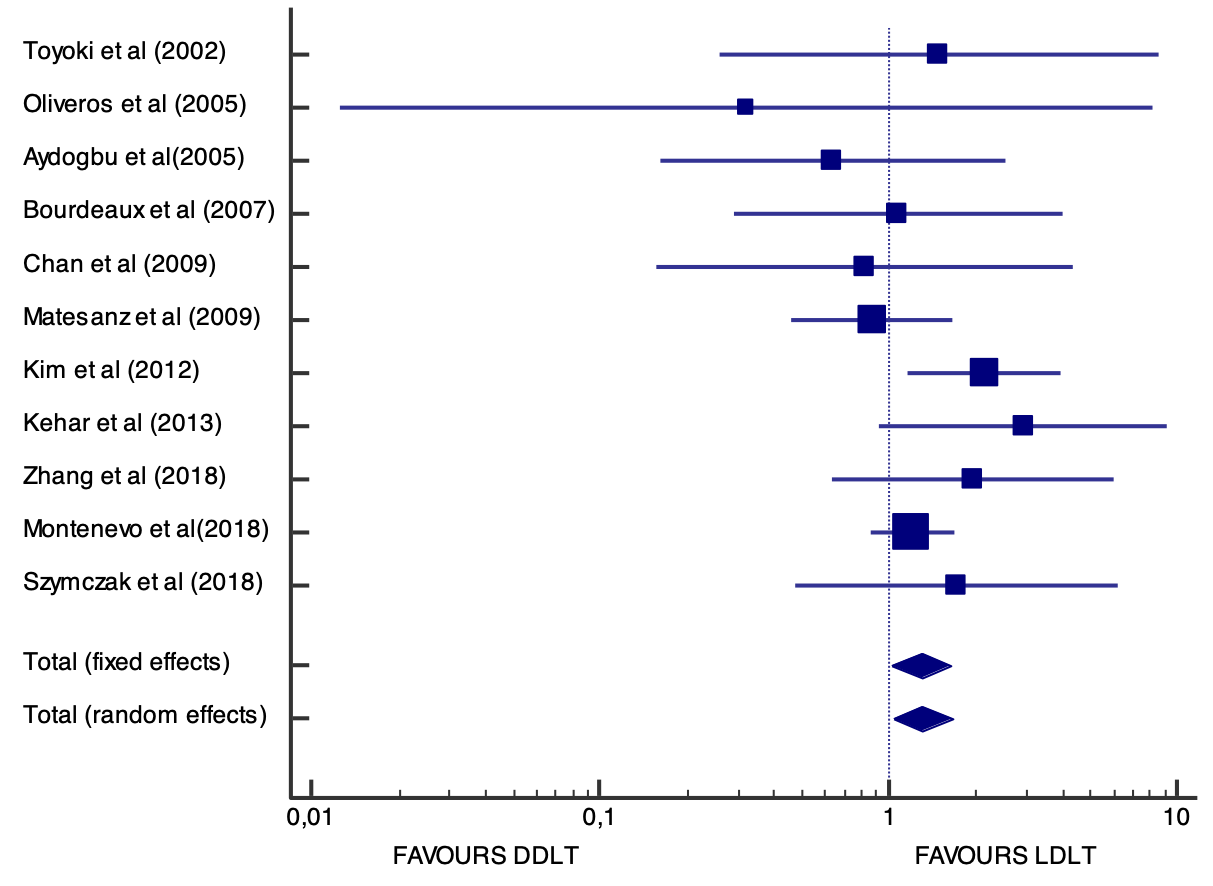
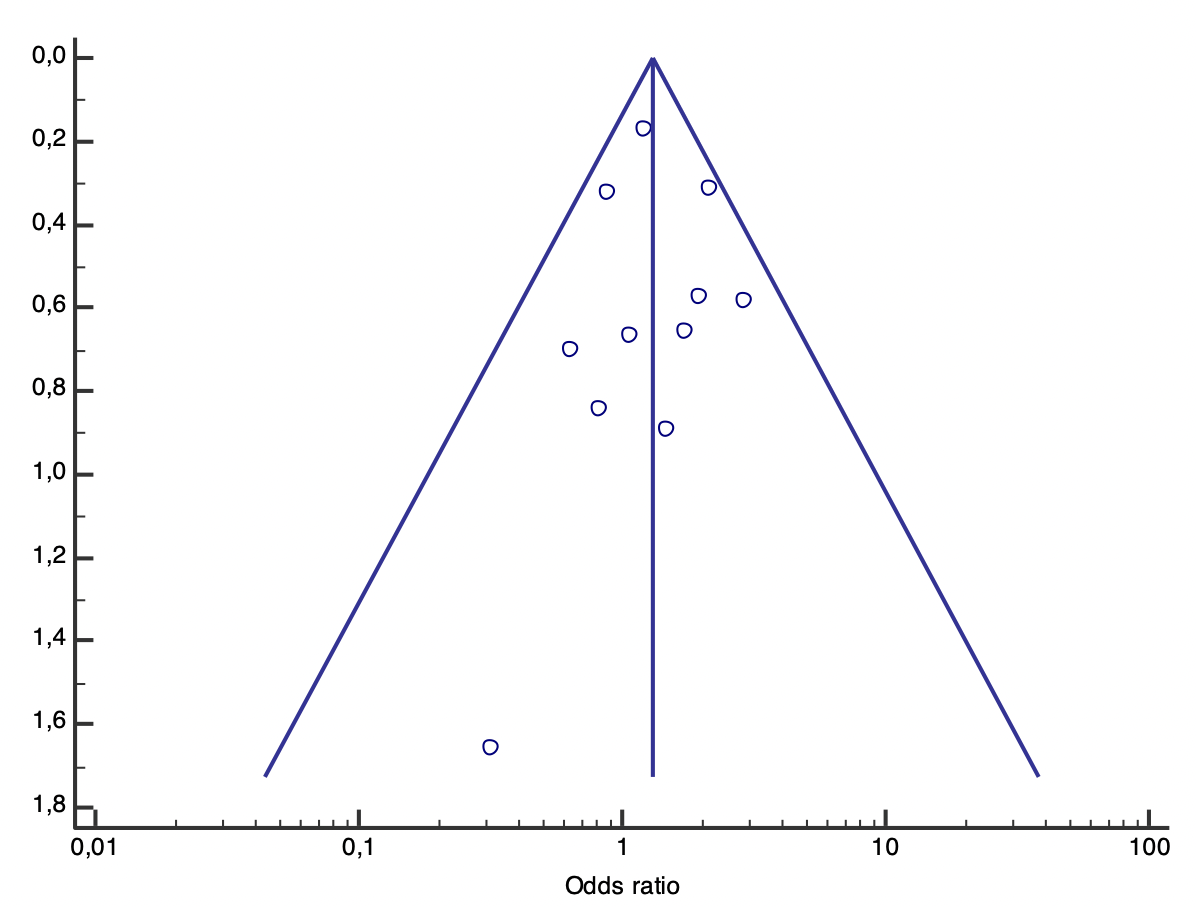
Materials and methods: The chosen study search formula was used on PubMed and Google Scholar. Cohort or case-control studies that reported one-year survival for both LDLT and DDLT were included. The year of publication was not an exclusion criterion. For the statistical analysis, the MedCalc 19 program was used, where the Forest Plot graphs were also made, as well as a Funnel plot for detecting heterogeneity.
Results: Out of a total of 2585 published articles obtained by applying the search formula, only 13 were classified for qualitative analysis and 11 for quantitative analysis. These 11 studies include 8445 patients under the age of 18 years. Of these, 1842 received a transplant from a living donor (LDLT) and 6551 received a transplant from a brain-dead donor (DDLT). From the point of view of heterogeneity, the Q value is 9.01 with a significance level p=0.53. The level of inconsistency is 0% with a confidence interval (0.00 and 56.6%). Of the 1842 children who received a transplant from a living donor, 1722 survived one year, and of the 6,551 children who received a transplant from a brain-dead donor, 6057 patients survived one year (plot pooled effect odds ratio=1,309 random effects).
Conclusion: In conclusion, for pediatric patients, receiving a transplant from a living donor is superior to that received from a brain-dead donor in terms of survival. Improving the anesthetic techniques, the intensive care techniques along with all the advances in complementary medication will lead to a better degree of survival in the coming years.