Dynamic kidney graft failure risk prediction using serial donor derived cell free DNA
Kexin Guo1, Lihui Zhao1, Steve Kleiboeker2, John Friedewald1.
1Comprehensive Transplant Center, Northwestern University, Chicago, IL, United States; 2Clinical Diagnostics, Eurofins Viracor, Lees Summit, MO, United States
Background: Donor-derived cell free DNA (ddcfDNA) has evolved as a non-invasive biomarker for monitoring kidney transplant patients for rejection. Trends in ddcfDNA over time may help predict important outcomes for the allograft. We examined samples from subjects enrolled in the CTOT08 clinical trial (NCT01289717) to determine the ability of joint modeling to dynamically predict graft survival in kidney transplant recipients.
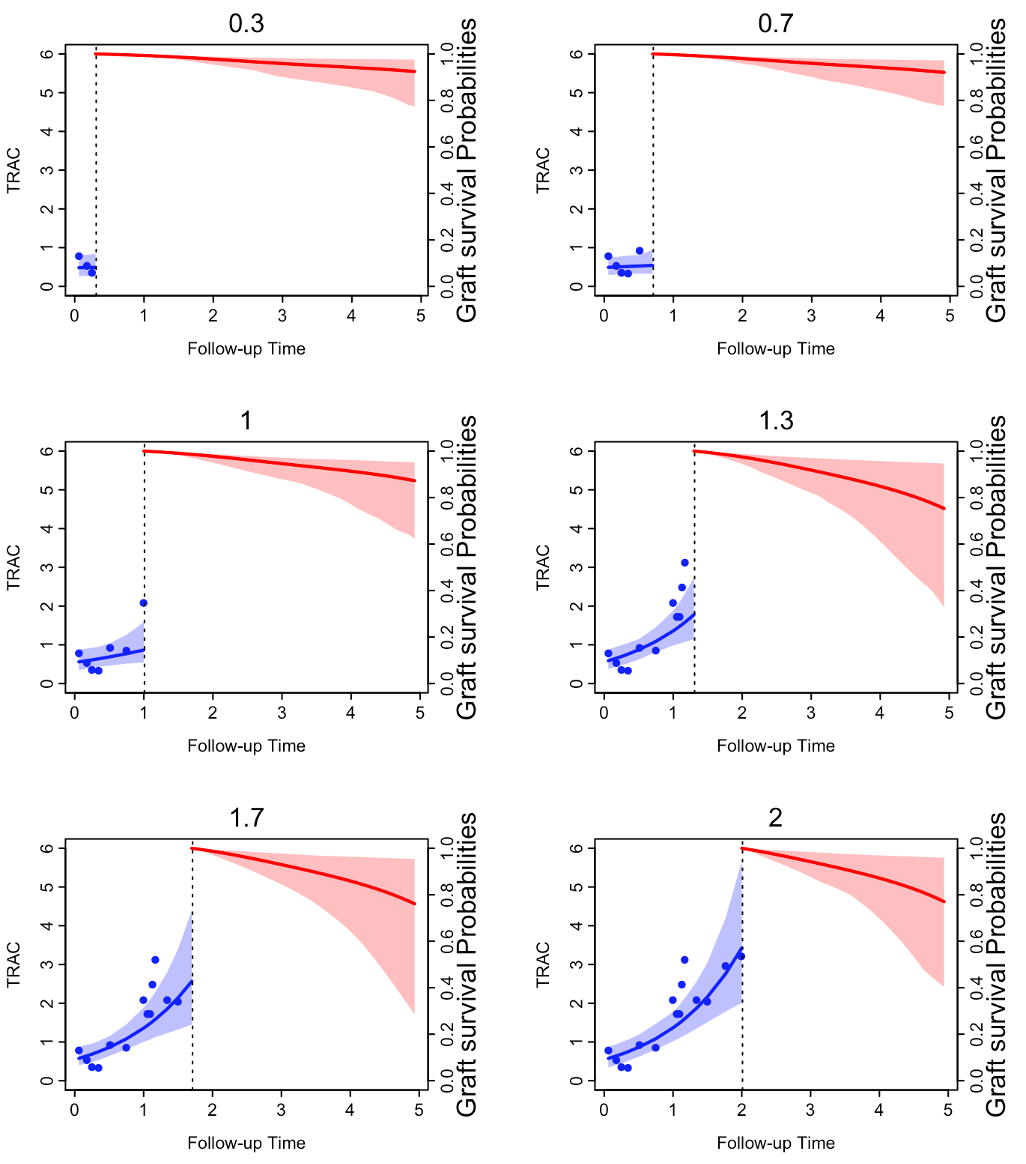
Methods: Serial blood samples collected in the first two years post-transplant were analyzed for ddcfDNA using the TRAC test (Eurofins – Viracor, Lees Summit, MO). We used joint modeling method to model the trend of serial ddcfDNA score to predict the 5- year death censored graft survival. We pre-defined 6 time points post-transplant and dynamically plotted two patients 5-year graft survival via the joint modeling method.
Results: Figures of predicted graft survival probability of two illustrative patient examples are presented below. Both patients have high 5-year graft survival probability based on their serial ddcfDNA scores up to 0.3-years post-transplant. Moving forward in time and follow up, the predicted probabilities start to diverge for these two patients. At the 2-year time point, for patient 1 with stable serial ddcfDNA scores, the predicted 5-year graft survival probability is 0.968 with 95% CI [0.918, 0.990].
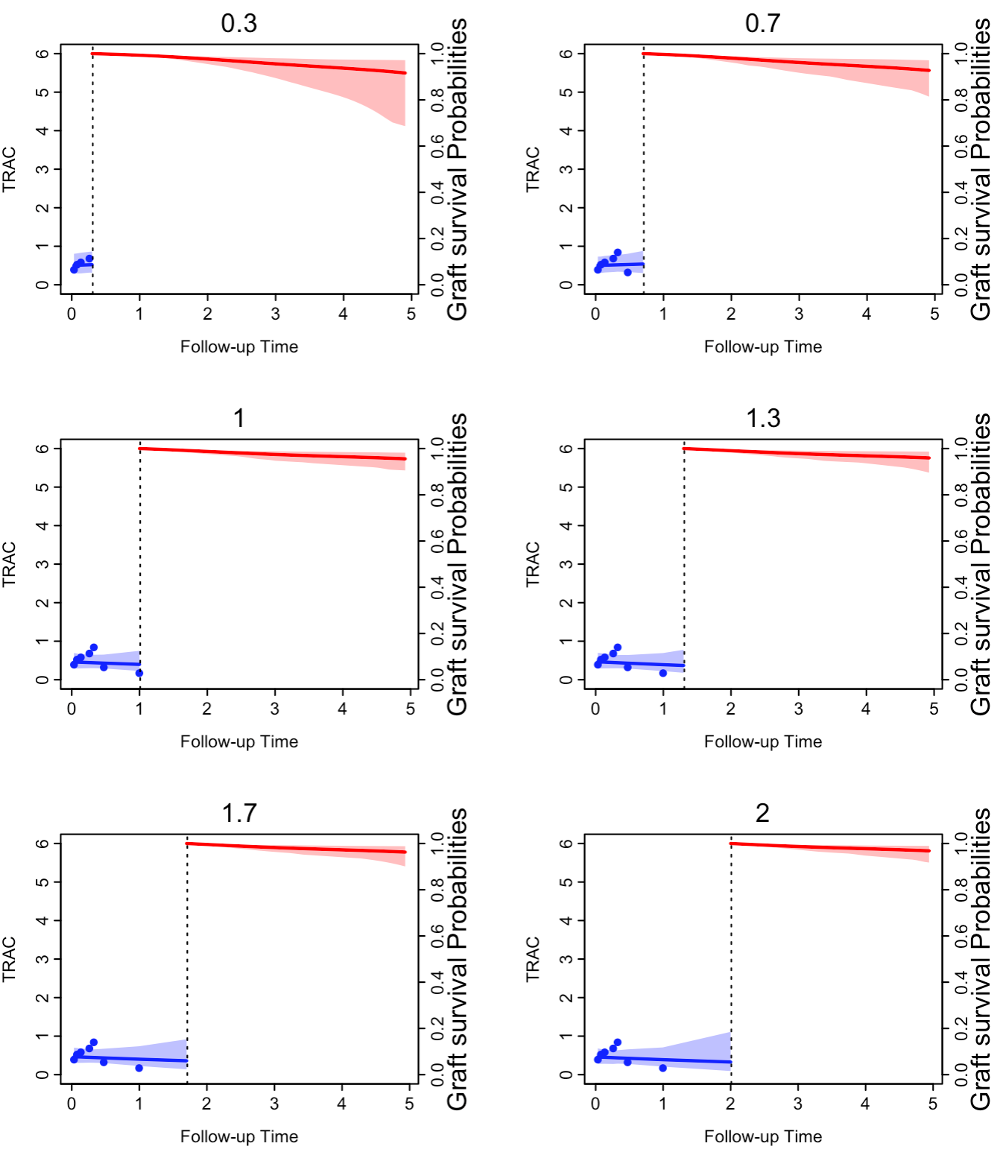
For the other patient (2) whose ddcfDNA scores continue to increase over time, the predicted 5-year graft survival probability is 0.770 with 95% CI [0.404, 0.959]. The second patient had a graft failure at 4.88 years post-transplant.
Discussion: Plasma ddcfDNA is evolving as both a diagnostic and a prognostic biomarker in the management of kidney transplant recipients. Using joint modeling, we were able to develop a dynamic risk prediction model for graft failure in patients. Future applications include further validation and eventually defined interventions to reduce the risk of graft loss.
