Comparable kidney transplant outcomes in selected patients with a BMI ≥40: a personalized medicine approach to recipient selection
Molly Jacobs3, Karanpreet Dhaliwal4, David Harriman5, Robert Stratta1, Alan Farney1, Giuseppe Orlando1, Jeffrey Rogers1, Amber Reeves-Daniel2, Colleen Jay1.
1Surgery, Abdominal Organ Transplant, Atrium Health Wake Forest Baptist Health, Winston-Salem, NC, United States; 2Nephrology, Atrium Health Wake Forest Baptist, Winston-Salem, NC, United States; 3Wake Forest School of Medicine, Winston-Salem, NC, United States; 4Cardiothoracic Surgery, University of Washington, Seattle, WA, United States; 5Urology, University of British Columbia, Vancouver, BC, Canada
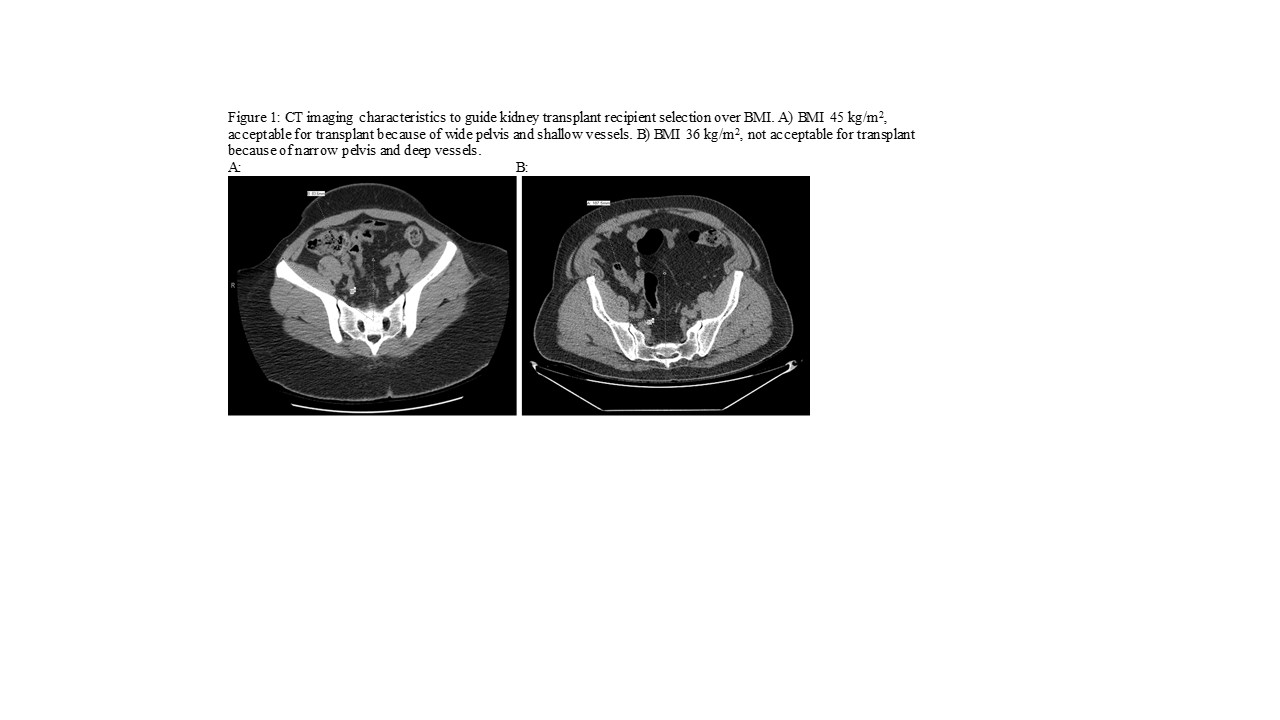
Introduction: Kidney transplantation confers a survival benefit compared with dialysis in most studies of obese patients. Yet, many transplant centers decline patients with a body mass index (BMI) ≥40 kg/m2. Our practice relies on computed tomography imaging to evaluate iliac depth and pelvic angle to assess candidacy (see Figure 1). Our aim was to evaluate post-transplant outcomes including survival in patients according to recipient BMI.
Methods: We performed a single-center retrospective review of adult kidney transplant alone recipients comparing BMI ≥40 patients (n=84, BMI =42±2 kg/m2) to a matched BMI <40 cohort (n=84, BMI =28±5 kg/m2). Patients were matched for recipient age, gender, race, presence of diabetes, and donor type (living vs. deceased).
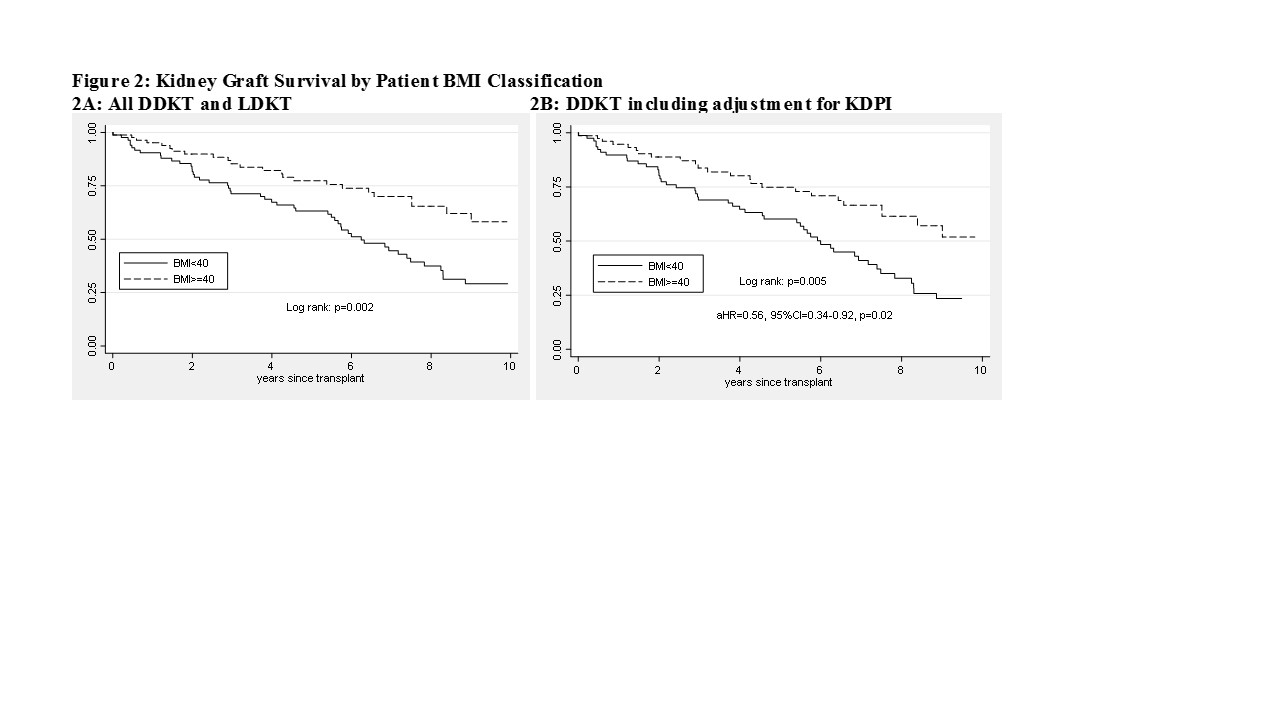
Results: BMI ≥40 patients were on dialysis longer pre-transplant (5.2±3.2 years vs. 4.1±3.5 years, p=0.03) and received lower kidney donor profile index (KDPI) kidneys (40±25% vs. 53±26%, p=0.003) compared to lower BMI patients. There were no significant differences in prevalence of delayed graft function, reoperations, readmissions, wound complications, patient survival, or renal function at 1 year according to serum creatinine and eGFR. Long-term graft survival was higher for BMI ≥40 patients, including after adjusting for KDPI (BMI ≥40: aHR=1.79, 95% CI=1.09-2.9) (see Figure 2). BMI ≥40 patients had similar weight gain and BMI change in the first year post-transplant (delta weight: BMI ≥40 +2.5±9.1 kg vs. BMI <40 +3.0±8.0 kg, p=0.74; delta BMI: BMI ≥40 +0.9±3.3 vs. BMI <40 +1.1±3.2, p=0.59). BMI ≥40 patients had a higher mean HbA1c level (6.9±1.7% vs. 5.9±1.4%, p=0.003) at one year post-transplant.
Conclusions: Overall patient survival and complications after kidney transplantation were comparable in BMI ≥40 patients compared to a matched cohort with lower BMI with improved long-term graft survival in the obese patients. BMI-based exclusion criteria for kidney transplantation should be reexamined in favor of a more individualized approach.