Kidney graft with vascular anatomical variants in a living donor transplant, 20 years of experience in a pediatric reference center
Alfonso Navarro-Gonzalez1, Monserrat Arreola-Gutiérrez1, Juan C Barrera-De León2, Mitzi R Becerra-Moscoso3, Eduardo Angulo-López1, Ana B Calderón-Alvarado3, María J Ruíz-López3.
1Transplant - Urology and Nephrology Department, Hospital de Pediatría CMNO IMSS, Guadalajara, , Mexico; 2Research and Teaching Department, Hospital de Pediatría CMNO IMSS, Guadalajara, , Mexico; 3Pediatric Surgery Department, Hospital de Pediatría CMNO IMSS, Guadalajara, , Mexico
Introduction: Achieving an ideal kidney graft (KG) for pediatric patients involves a convoluted process. Their chances of survival are reduced by an extended waiting list; leading the need to include KG with vascular anatomical variants to maximize the donor pool and face the existing demand. Such is the case of grafts with multiple renal arteries (MRA) which are a subject of debate that have contradictory results. We present 20 years of experience in KG transplantation with MRA, in a pediatric reference hospital center.
Method: A cross sectional study was conducted. The data of the living donor (LD) consultation from 2001-2021 were analyzed, all KG donors were included in the LD program with MRA and their relationship with the evolution of the donor. We analyzed surgery time, warm ischemia time, bench surgery (BS), donor hospital stay and post-surgical vascular complications in the KG. Descriptive and inferential statistics were obtained using statistical program SPSS 25.0, chi square for proportions and Student's t-test for means.
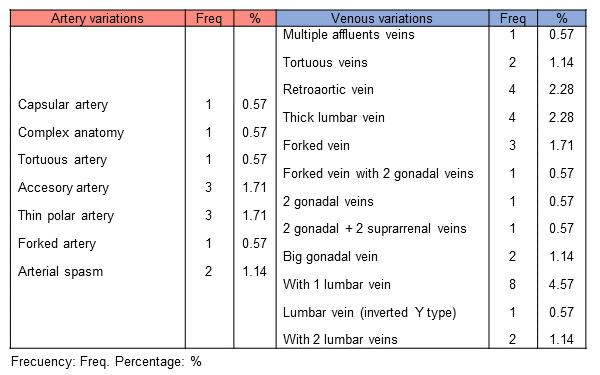
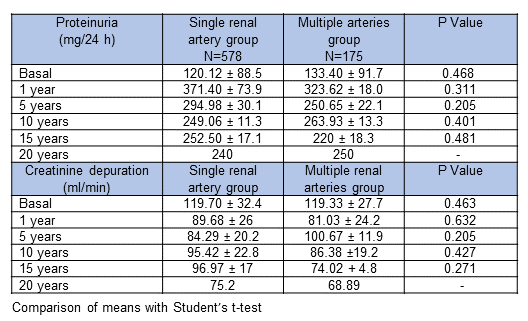
Results: In this period 753 patients were evaluated, 175 (23%) MRA grafts were transplanted due to complexity of the contralateral kidney. In 9 (5.1%) of them a right nephrectomy and 166 (94.8%) a left nephrectomy were performed for LD. 151 KG had 2 renal arteries, 23 KG had 3 renal arteries and 1 KG had 4 renal arteries. 131 KG had BS and the rest had vascular anastomosis without BS. Mean surgery time was 87.4 + 23.9 min (p=0.000), with mean warm ischemia time 217.8 + 91.2 min (p=0.000). Main surgical findings were 30 (17.1%) cases of venous variants like lumbar vein, retroaortic veins, forked or tortuous veins. 12 cases (6.8%) were arterial variants like accessory arteries, thin, forked or tortuous arteries. There were no complications in 74.2% of nephrectomies. Most common complications were pleural or retroperitoneal opening (14.8%), lumbar vein laceration (1.7%), renal artery injury (1.7%) and degloving of the renal capsule (2.2%). Mean hospital stay was 2.89 + 2.3 days (p=0.004). The long-term follow up with proteinuria and creatinine depuration levels was similar to single renal artery group.
Conclusion: MRA transplantation is a safe option for donors with similar results to single-artery transplantation in short such in long term. Even though there are significant difference in surgery time, warms ischemia time and hospital stay, the complications associated with the MRA graft are not different from single-vessel graft; considering all nephrectomies were realized only by one surgeon. We conclude that MRA is not a contraindication for renal transplantation in living donors.