Prediction of acute rejection post-kidney transplant: an artificial intelligence approach
Hatem Ali1, Mahmoud Mohammed3, Bernard Burke4, David Briggs2, Nithya Krishnan1.
1Renal department, University Hospitals of Coventry and Warwickshire, Coventry, United Kingdom; 2NHSBT, Birmingham, United Kingdom; 3University Hospitals of Mississippi, Mississippi, United States; 4Research Centre for Sport, Exercise and Life Sciences, Coventry University, Coventry, United Kingdom
Background and Aims: Acute rejection is one of the major risk factors that affects the outcome of kidney transplant. Several immunotherapy protocols have been implemented to prevent acute rejection and improve outcomes. The aim of our study is to use artificial intelligence to build a prediction model for acute rejection episodes in the Tacrolimus era.
Method: All kidney transplant patients registered in UNOS database between 1st of January 2005 and 1st of December 2019 were retrospectively reviewed. Inclusion criteria: deceased donor transplants that were discharged on Tacrolimus/Mycophenolate Mofetil. Exclusion criteria: multiple organ transplants, previous kidney transplants, recipient age<18 years old, living donor transplants, patients not discharged on Tacrolimus/Mycophenolate Mofetil immunotherapy, missing HLA mismatch or ABO incompatible transplant. Patients with complete data were included in the analysis. We performed a CART (classification and regression tree) analysis to build a decision tree for prediction of acute rejection at six months post-transplant. The model evaluation criterion was to maximise recall and minimize false negative prediction. We divided the dataset into training and testing data based on random selection (ratio 70:30). Variables included in the analysis were: recipient characteristics (age, sex, BMI, ethnicity, diabetes, recipient/donor CMV status, time spent on dialysis), donor characteristics (KDPI score) and transplant characteristics (type of induction therapy, steroid therapy at time of discharge, cold ischemia time, delayed graft function, PRA, HLA-A, B,DR, and DQ mismatch). We performed a cost complexity pruning to treat overfitting of the decision tree. We determined the best set of alpha for pruning using optimized cross-validated grid-search for hyperparameter tuning. We created the model where we get highest train and test recall. Feature importance scores were calculated on the weighted Gini indices.
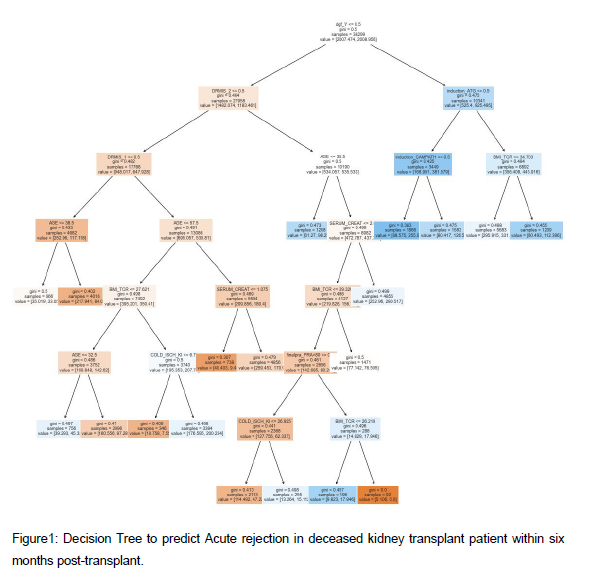
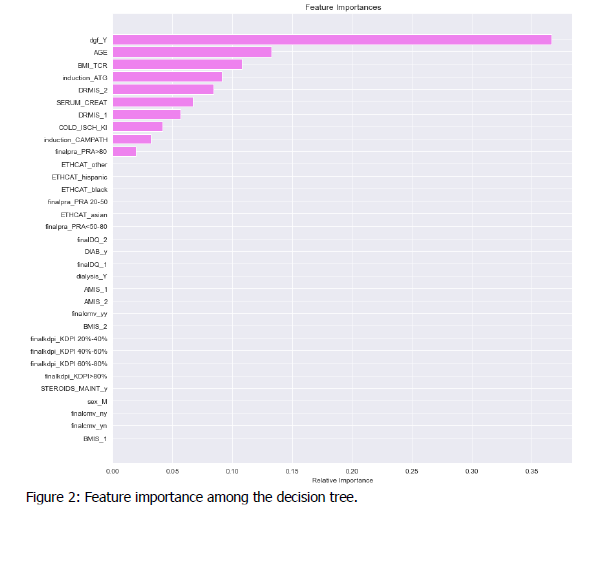
Results: 54,714 patients were included in our study. Figure 1 shows the results of our decision tree. The decision tree recall score was 73.8% in the training data and 66.3% in the test data. Figure 2 shows the feature importance among the decision tree. The most important feature was occurrence of delayed graft function (Relative importance=0.40), followed by age (relative importance=0.14), body mass index (relative importance=0.11), induction with Anti-thymocyte globulin (relative importance=0.8) and 2-HLA-DR mismatch (relative importance=0.7).
Conclusion: Artificial intelligence and decision trees are promising tools to predict the outcomes of kidney transplantation. Delayed graft function, age, type of induction therapy, and HL-DR mismatches are key players in the decision tree to predict acute rejection.