What about the heroes? Living donor liver outcomes, from a single Latin-American center experience between 2009-2022
Leonardo Montes1, Dario Teran Dr1, Andres Fraile Dr1, Florencia Fernandez Dra.1, Valeria Descalzi Dra.1, Laura Reyes Toso Dra.1, Pablo Farinelli Dr1, Pablo Barros Dr1, Gabriel Gondolesi Dr1.
1Hepato pancreato biliary surgery , Fundacion Favaloro, Buenos Aires, Argentina
Background: The shortage of organs favors the need for considering the use of living donor´s grafts (LD) for liver transplantation (LT). Reports on long term donor outcomes are scarce. Our aim was to report the long term postoperative outcomes of all LD done in our center.
Materials and methods: Retrospective observational study from 41 consecutive LD surgeries performed between 2009 and 2022 in a single center. Variables included were: donor (D) demographics, transplant indications, D-Recipient relationship, type of transplant, surgical approach, type of graft, operative time, days in ICU, length of hospital stay, graft weigh, estimated volume, graft/weight ratio (GRWR), postoperative complications using the Dindo- Clavien (DC) classification and mortality. As part of the evaluation, liver anatomy and volumetric assessment was done using CT-Scan and MRI. Biliary anatomy was studied with intraoperative cholangiography. Parenchymal transection was performed using CUSA. Statistical analyses were performed using SPSS v20.0.
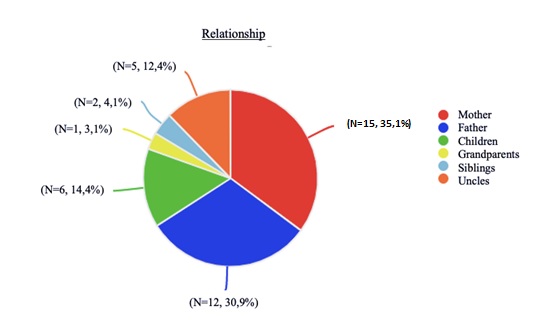
Results: Twenty four patients (58%) were woman. The mean donor age was 30(±7) years. Transplant indications were biliary atresia (N: 19, 46.3%); Alagille´s syndrome (N: 5, 12.2%), fulminant liver failure (N:5, 12.4%), primary biliary cholangitis (N:4, 9.8%), cryptogenic cirrhosis (N:2, 4.9%), colorectal CA liver metastasis (N:1, 2.4%), and others (N:5,12%). In 63% of cases the donors were parents, figure. Type of transplant was Adult-Pediatric (N: 35, 85%) and Adult-Adult (N: 6, 14%). Open surgery was used in (N: 38, 92%); using median laparotomy in 80% of cases (N: 33), 3 were hand assisted. Types of graft were: left lateral seccionectomy (N: 27, 66%), left lobe (N: 11, 26%) and right lobe (N:3, 8%). The median operative time was 302 (130-570) minutes. Mean graft weight was 309±177 grs, while the mean graft estimated volume calculated with the preoperative CT-Scan was of 342±174gr. Mean GRWR was 2.8±2. The overall complications rate was 12% (N: 5); minor complications were: intra-abdominal collections (N: 2, 4.9%; DC: IIIa and I), biliary fistula (N: 1, 2.4%; DC: I); while major complications were: one hemoperitoneum (DC IIIb) and one pyloric syndrome (DC IVa); all occurred within the first 30 pop. days. Mean ICU stay was 1±0.4 days; length hospital stay was 3±1 days. No postoperative deaths were observed.
Conclusions: LD liver transplantation remains as a complex procedure, but the evolving experience, the sustained deficit of cadaveric organs, together with an acceptable morbidity, increases the team willingness to consider its use, in order to reduce the mortality in the waiting list.
