Validating survival scores following liver re-transplantation, at a single center
Leonardo Montes1, Andres Fraile Dr1, Florencia Fernandez Dra.1, Dario Teran Dr1, Laura Reyes Toso Dra.1, Diego Ramisch Dr1, Silvina Yantorno Dra.1, Pablo Barros Schelotto Dr1, Valeria Descalzi Dra.1, Gabriel Gondolesi Dr1.
1Hepato pancreato biliary surgery , Fundacion Favaloro, Buenos Aires, Argentina
Introduction: Liver re-transplantation (reTx) is the only therapeutic option for irreversible liver-graft failure, with a reported frequency between 3 and 24%. A strict patient selection is mandatory due to the high risk of the procedure. Our aims were to: 1) evaluate the prevalence and outcomes of reTx at our centre; 2) identify survival predictor factors, validating reported mortality predictor scores for urgent, early and late reTx.
Patients and Methods: From July 1995 to March 2022, 1001 consecutive adult liver transplants were performed at our center. Demographical and clinical variables, second graft survival and survival predictor scores (Rosen modified, UCLA and Markmann) were retrospectively applied and analysed for urgent, early and late reTx (2nd and 3rd reTx were excluded). Urgent reTx (U-reTx) was defined as those done within 7 days, early reTx (E-reTx) between 8 and 30 post-operative days, late re-Tx (L-reTx) those that occur after. Statistics: univariate and multivariate analysis, logistic regression for mortality, using ROC curves. Kaplan Meier and log rank for actuarial survival were performed in SPSS v20.0.
Results: Sixty-nine reTx (6.8%) were done; mean age was 39±17 years; 58% males. Five (8%) were U-reTx, eight (11%) were E-reTx and 56 (81%) were L-reTx. The mean time between primary LTx (p-LTx) and U-reTx and E- reTx was 4±2 and 26±14 days, respectively and 2016±240 days between p-LTx and L-reTx. Main causes for U-reTx were arterial thrombosis (AT) =3 and primary non function (PNF) =2, causes for E-reTx were AT =5 and PNF =3. L-reTx was indicated due to recurrence disease: 15 (HCV 9, HBV 2, and HAI 4), ductopenic rejection=15, biliary complications= 10, Ischemic cholangiopathy = 9, AT=7. Mean donor age was 35±13 year. Two variables were found to be independently associated with poor outcome, recipient age >45 years (odds ratio 4.1, 95% CI 1.5 to 11.4; p=0.006), and cold ischemia time (CIT) >495 minutes (odds ratio 4.4, 95% CI 1.4 to 13.3; p=0.009). Overall, U-reTx, E-reTx and L-reTx graft and patient survivals at 1, 5 and 7 years are shown in figure 1, as well as those with p-LTx. Markmann survival score was the most sensitive and specific in our cohort (Figure 2).

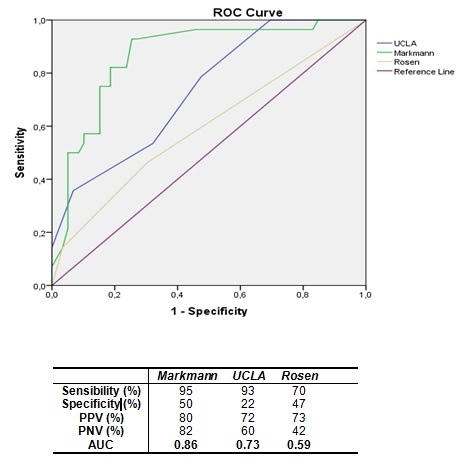
Conclusions: Liver reTx has become an option for patients with early and late graft failure. Recipient age >45 and CIT > 495 minutes were associated with worse outcome. Markmann predicting score was the most useful tool to predict poor outcome in our cohort.
