Teratoma in transplanted patient, case report and review
Luis Garcia1,2, Lionel Vargas1, Diana Fernandez1, Dario Cantu1, Sandra Gutierrez1, Karla Manrique1, Aldo Garcia1, Lourdes Quintero3.
1Surgery, Hospital General de Mexico Dr. Eduardo Liceaga, Ciudad de Mexico, , Mexico; 2Surgery, Hospital Especialidades CMN SXXI IMSS, Ciudad de Mexico, , Mexico; 3Pathology, Hospital General de Mexico Dr. Eduardo Liceaga, Ciudad de Mexico, , Mexico
Background: Compared with the general population, a transplant patient has a 10-fold higher incidence of developing a de novo neoplasm. Added to the common factors of the general population are immunosuppression, or the existence of oncoviruses.
Methodology: We describe the case of a 59-year-old male, group B+, who received a transplant from a Related Living Donor in 2011, sharing a haplotype, undergoing induction with Daclizumab 80mg DU, and with immunosuppression based on Cyclosporine 1.8mg every 12h, Mycophenolate 1g every 12 hours and Prednisone 5 mg every 24 hours; He began suffering in December 2020 with abdominal pain in the epigastrium, hyporexia and weight loss, Laboratories: Creatinine: 1.15, Urea 32, Glucose 102mg / dL, Hb 17.6mg / dL, Hto 52.40, Leukocytes 7.9X1000, Platelets 233x1000; tumor markers: Alpha fetus 2.16 ng/ml, CA 19-9 524.5 IU/ml, A. Carcinoembryonic 67.53 ng/ml. On examination, the kidney graft showed no alterations, and a palpable abdominal tumor of 30 x 25 cm, painful on palpation. Tomography reported a retroperitoneal tumor of 25.8 x 16.9 x 19 cm with displacement of adjacent structures and compression of the inferior vena cava.
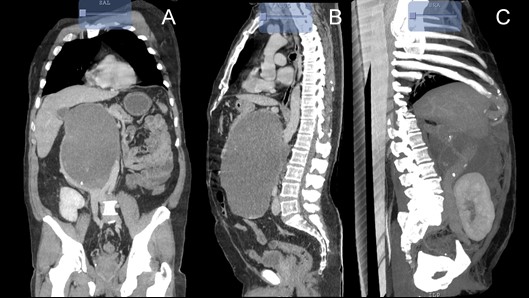
Resection of the tumor is performed, finding: Retroperitoneal tumor of 25 x 25 x 20 cm on the vena cava and aorta, which displaces the pancreas towards the head, without its involvement, with a mucous content of 2 Lts.

At one month of follow-up with creatinine 0.94, Hb 12.2, Hct 36.4, plaq. 284, leukocytes 6.0. With tolerance to the oral route, without pain, and definitive histological report compatible with Retroperitoneal Mature Teratoma.
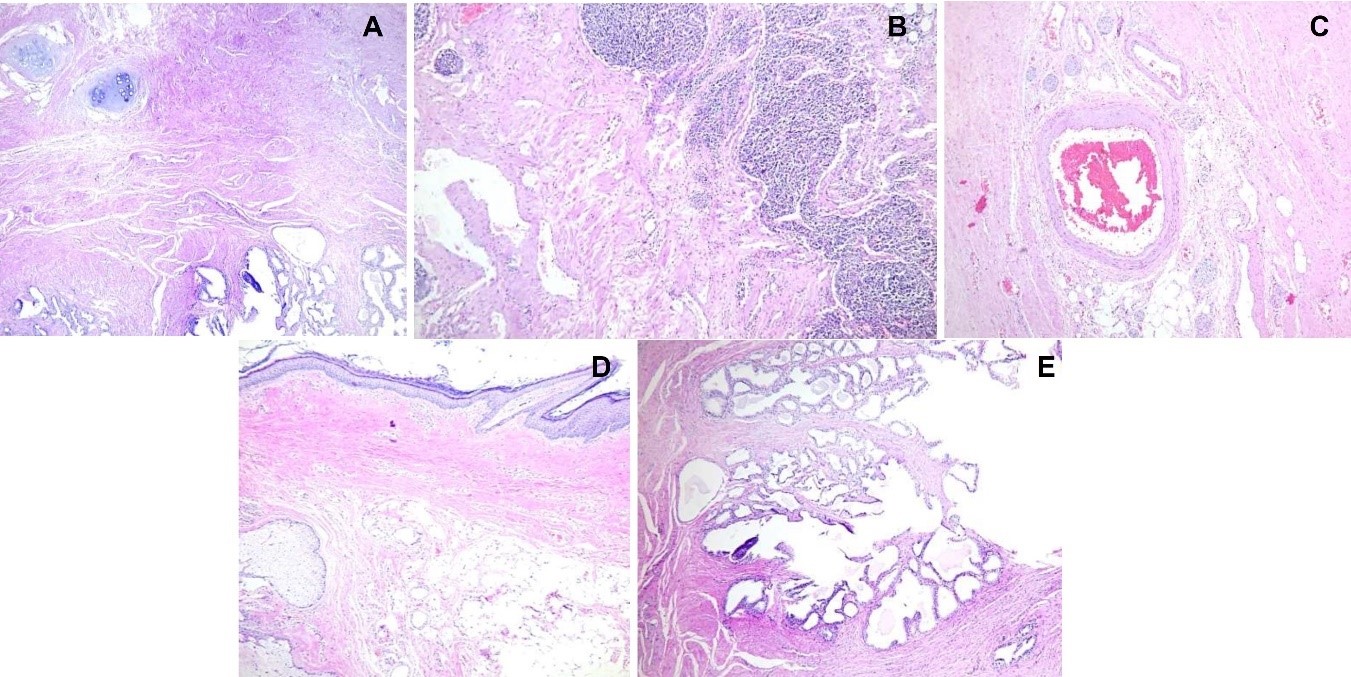
Discussion: Primary mature teratomas are rare nonseminomatous germ cell tumors of well-differentiated parenchymal tissues composed of somatic cell types, more common in childhood and rarely in adults where it represents 1 to 11% of retroperitoneal tumors, more frequently in women in a 3:1 ratio and are usually located near the upper pole of the kidney, more frequently on the left side, or in structures in midline. Retroperitoneal teratomas represent only 4% of all primary teratomas. Only a few case reports have been documented in the literature. Serum markers, such as CA19.9, CEA and AFP, may be elevated. The rate of malignancy in adults is 26% and increases with age, male sex, and the presence of immature tissues and solid components. Surgical resection is the mainstay in the treatment. Although mature teratomas are benign, malignant transformation occurs in 3-6%. The prognosis after complete resection has a five-year survival rate of 100%.
Conclusions: Mature primary retroperitoneal teratomas very rarely occur in adult male patients and are usually asymptomatic. The definitive diagnosis is established after histological evaluation. Surgical resection is the main treatment to evaluate if there are immature and solid elements that need long-term follow-up due to the increased risk of malignancy.
