Outcome of 250 lung transplants in Saudi Arabia, 92% marginal donors
Mohamed Hussein1,2, Norberto R. Santana1, Waleed Saleh1, Mahmoud Y. Hashim1,3, Rayid Abdulqawi1, Eid Almutairy1.
1Lung Health Center- Organ Transplant Center, King Faisal Specialist Hospital and Research Center, Riyadh, Saudi Arabia; 2Cardiothoracic Surgery, Ain Shams University, Cairo, Egypt; 3Cardiothoracic Surgery, Helwan University, Cairo, Egypt
Purpose: A total of 250 lung transplantations (LTx) were performed at a single center in Saudi Arabia. 92% of our donors are marginal. The criteria of deceased brain dead donors represent unique differences that bring unique challenges. This report highlights the challenges, management strategies and outcomes.
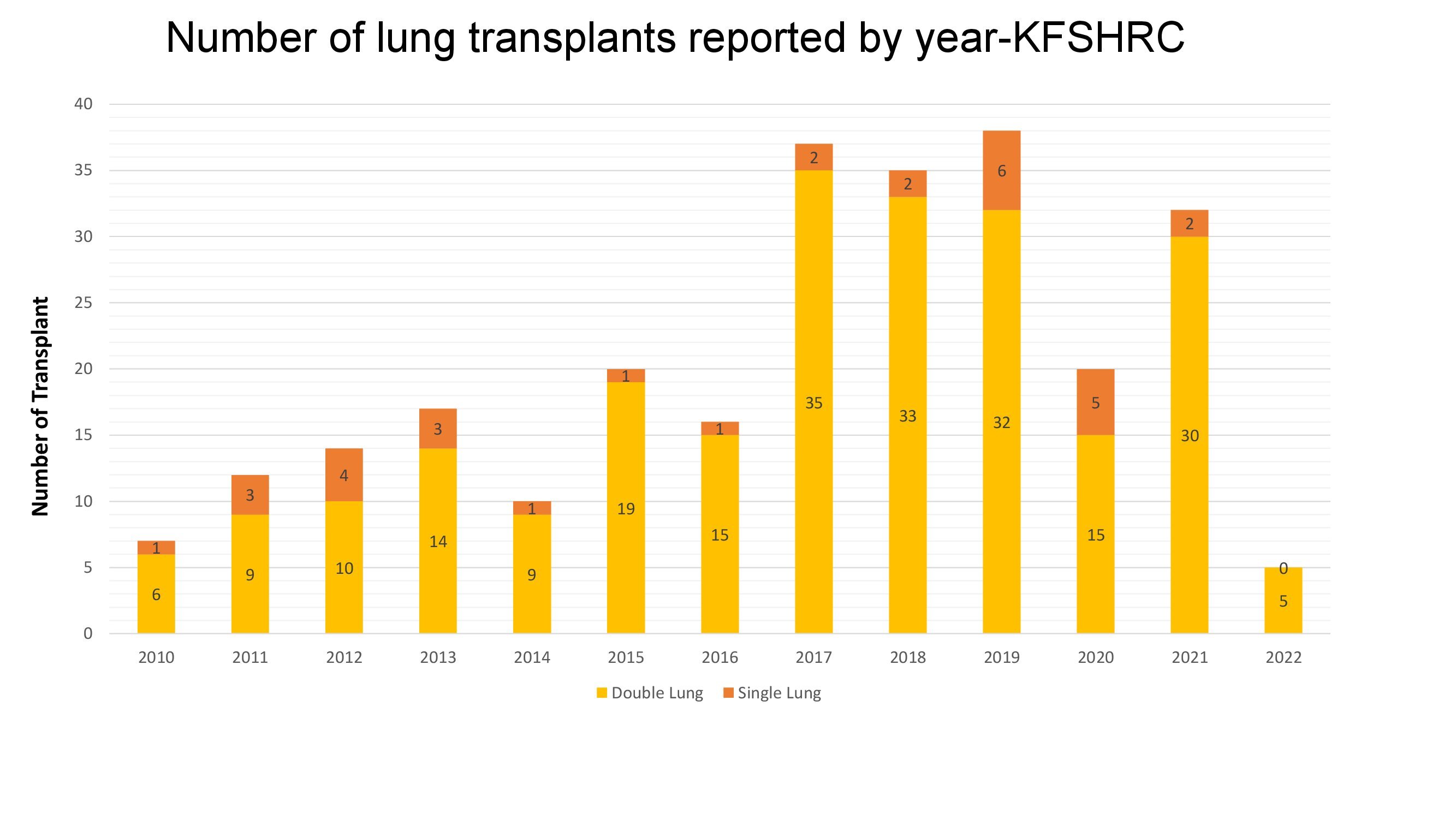
Methods: The LTx Program at King Faisal specialist hospital was established in 2000 as the first and only active program in Arabian countries. Over the last 12 years the program has witnessed rapid growth. Retrospective review of 250 patients and their donors that underwent LTx at our center between January 2000 and February 2022.
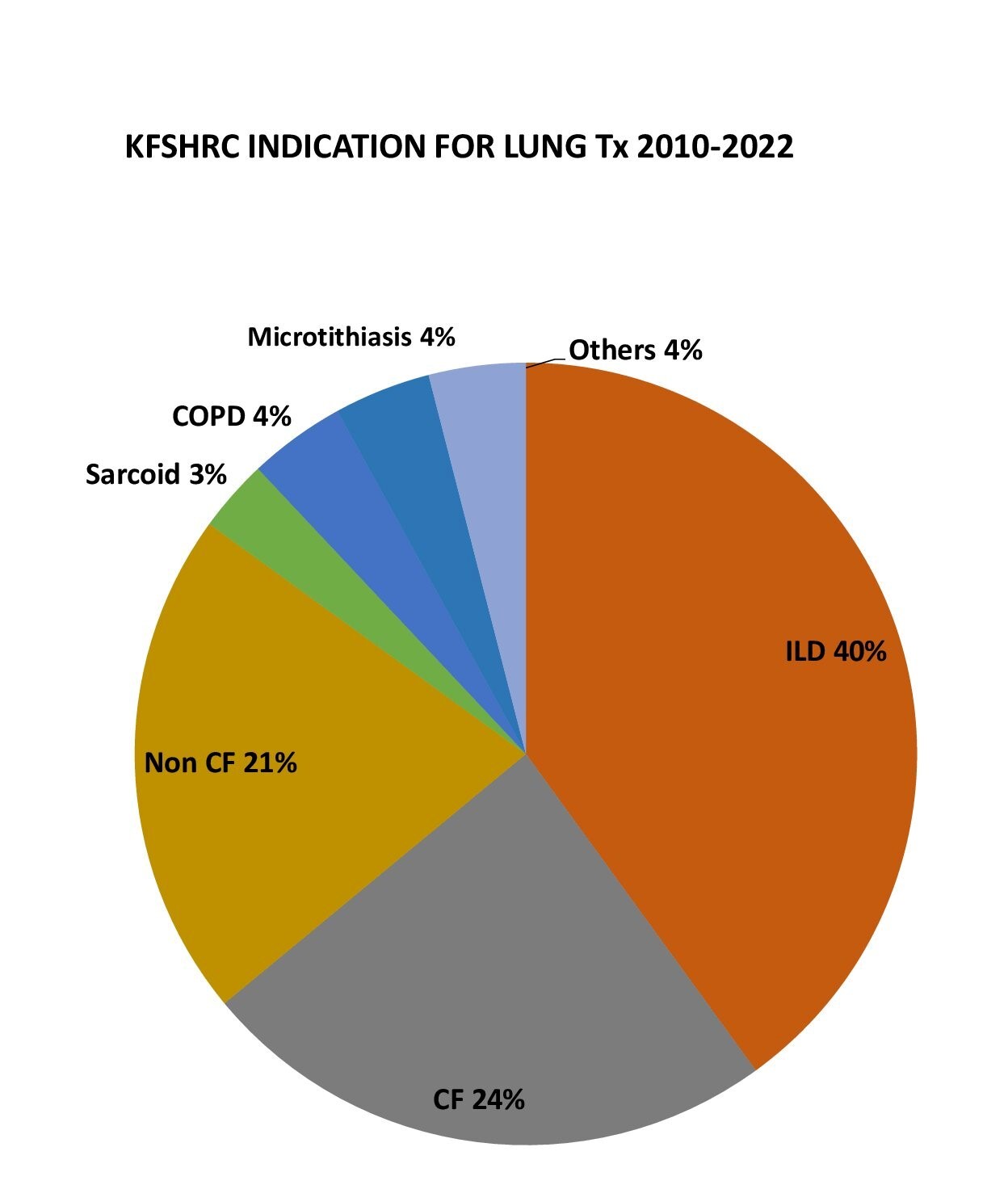
Results: The most common indication for LTx was pulmonary fibrosis (40%), followed by cystic fibrosis (CF)-related bronchiectasis (24%), non-CF-related bronchiectasis (21%), chronic obstructive pulmonary disease (4%), sarcoidosis (3%), Microtithiasis (3%). The indications in other patients included pulmonary capillary hemangiomatosis, lymphangioleiomyomatosis, and retransplantation.
Only 39% of our lung transplant recipients had a normal BMI of 18–28 kg/m2, whereas 61% were either underweight with a BMI of <18 kg/m2 (42%) or overweight with a BMI of >28 kg/m2 (19%).
Regarding Lung donors (LDs) 92% of our lungs were marginal. 10% age>55 years, 16% PO2 < 300 mmhg, 32% abnormal CXR, 22% Purulent secretions on bronchoscopy, 83% Prolonged ventilation more than 5 days with a mean duration of mechanical ventilation (MV) of 9+/-7 (days).
Bacterial colonization was noted in 74% of LDs, including multidrug-resistant bacteria such as acinetobacter (31%), klibsiellae (24%) and pseudomonas (12%).
Size missmach was a challenge, 72% required lung volume reduction. In 9 cases bilateral lower lobar Tx, a unilateral lobarTx with contralateral whole lung in 15 cases, the rest required lung trimming.
Over the last 7 years extracorporeal membrane oxygenation (ECMO), was used in 24% of our LTx as a rescue strategy for grade 3 primary graft dysfunction with 30 days survival of 92% and 1 year survival 88%.
Ex vivo lung perfusion was used to expand our pool of LDs, 11 successful cases from 23 attempts were performed over the last 5 years.
In spite of the liberal utilization of marginal donors and prolonged post lung transplantation mechanical ventilation {Median (range)}11 (1-145 days), length of ICU stay 14 (3-145) and length of hospital stay 36 (12-168), our 30 days, 90 days, 1 year, 3 years and 5 year survival rates were 94.3%, 89%, 87.5%, 76% and 62.5% respectively.
Conclusion: Shortage of good donors forced us to use extended criteria to transplant high risk patients. The selective use of Ex vivo and ECMO helped to achieve comparable results. Prolonged ventilated donors even with bacterial colonization can be utilized for LTx, size mismatch can be overcome by different surgical techniques.


right-click to download
