Cost-effectiveness of interventions to increase utilization of kidneys from deceased donors with primary brain malignancy in an Australian setting
James Hedley1, Karan Shah2, Melanie Wyld1,3, Rachael Morton2, Juliet Byrnes1, Brenda M Rosales1, Nicole L De La Mata1, Patrick J Kelly1, Kate Wyburn1,4, Angela C Webster1,2,3.
1Collaborative Centre for Organ Donation Evidence, University of Sydney, Sydney, Australia; 2National Health and Medical Research Council Clinical Trials Centre, University of Sydney, Sydney, Australia; 3Centre for Transplant and Renal Research, Westmead Hospital, Sydney, Australia; 4Renal Unit, Royal Prince Alfred Hospital, Sydney, Australia
Introduction: Kidneys from potential deceased donors with brain cancer are often foregone due to concerns of transmission risk to recipients. This may be due to uncertainty around donors' medical history and their absolute transmission risk, or risk-averse decision-making among clinicians. However, transmissions are rare and prolonging waiting time for recipients is harmful.
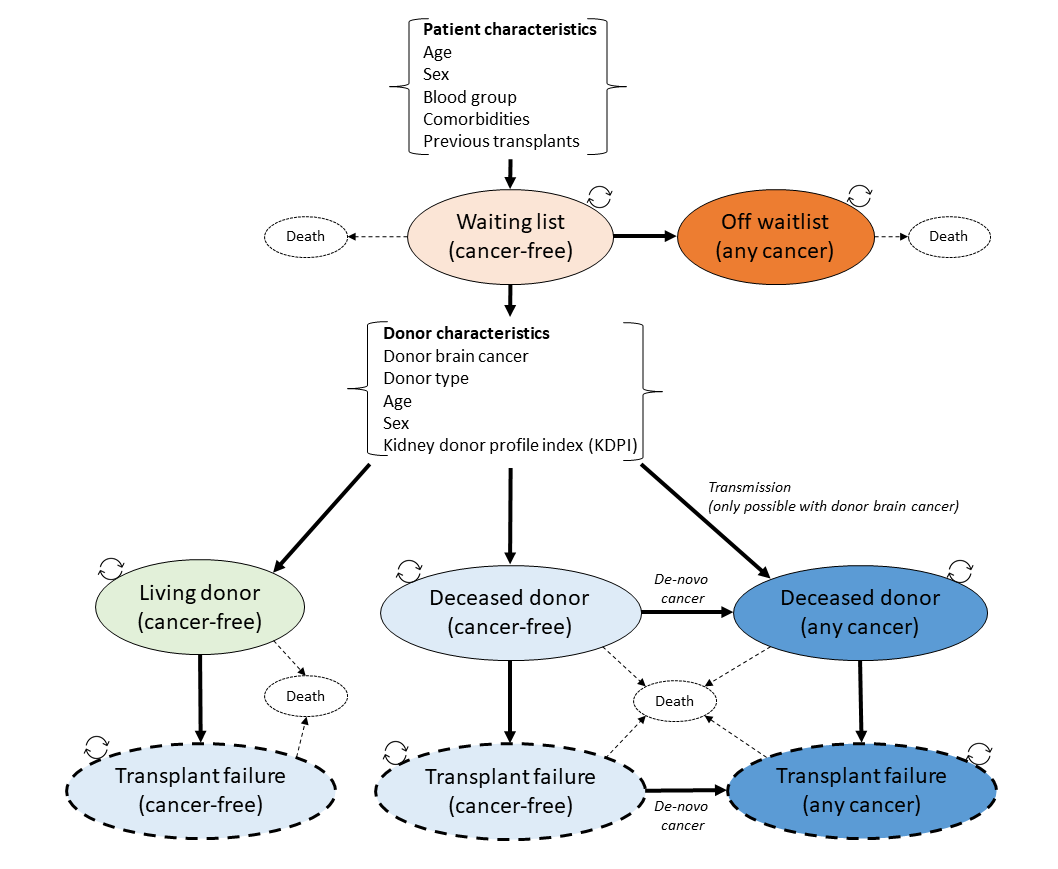
Method: We assessed the cost-effectiveness of increasing utilization of these potential donors using a Markov model patient simulation (Figure 1) to estimate costs and consequences from a payer perspective (Australian government) using linked transplant registry data. We estimated costs and quality-adjusted life-years (QALYs) from three interventions: decision support for clinicians in assessing donor risk, improved data accuracy with real-time data-linkage to hospital records and cancer registries, and increased risk-tolerance to allow intermediate-risk donors.
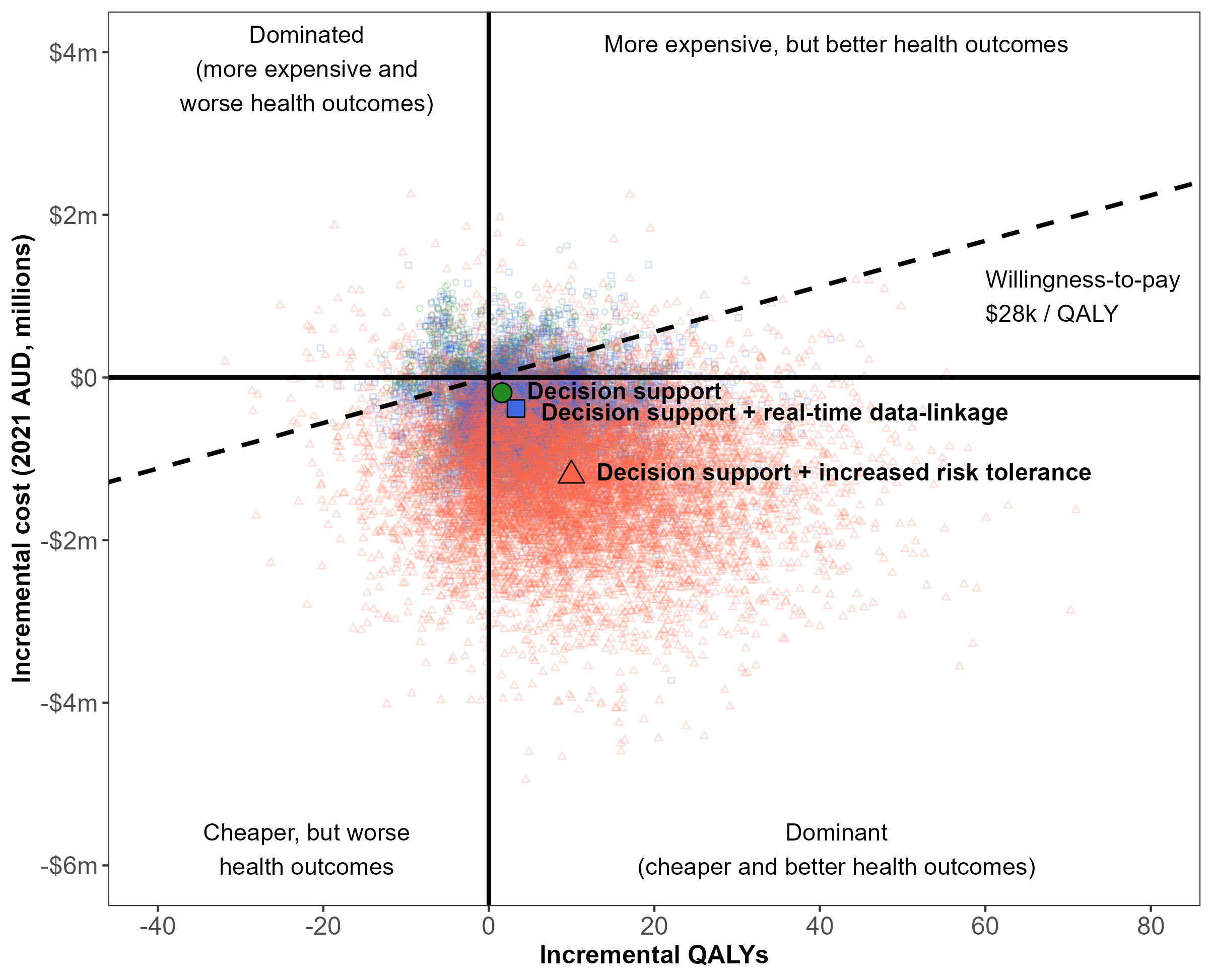
Results: Decision support increased donation 0.3% with a 2% transmission rate and was dominant (improved QALYs and cost-saving) in 56% of simulations (Figure 2). Real-time data-linkage increased donation 0.6% with 1.8% transmissions and was dominant in 57% of simulations. Increasing risk tolerance increased donation by 2.1% with 3.3% transmissions and was dominant in 75% of simulations (mean +10.0 QALYs and $1.2m ($904k USD) cost-savings).
Conclusion: Accepting intermediate-risk donors with brain cancer is likely to improve patient outcomes and reduce overall healthcare expenditure.
This work was funded by a National Health and Medical Research Council Postgraduate Research Scholarship (APP1191066).

right-click to download
