
Pancreas transplantation from cardiac death donors versus neurological death donors at a tertiary care center
Catherine Parmentier1, Michael Bleszynski1, Samrat Ray1, Andrea Norgate1, Gonzalo Sapisochin1, Ian McGilvray1, Anila Yousuf1, Markus Selzner1, Trevor Reichman1.
1Multi Organ Transplant Department, University Health Network - Toronto General Hospital, Toronto, ON, Canada
Introduction: Pancreas transplantation is the only curative treatment for patients with complicated diabetes. Donor organ shortages and strict organ allocation policies are rate limiting factors that limit potential recipients from receiving a graft. The pancreas is also the most discarded organ for transplantation further limiting suitable grafts for transplant. To meet the demands of the organ shortage, expanding the criteria for suitable pancreas donors has been explored. The program in Toronto has been using donation by cardiac death (DCD) pancreas donors for over a decade.
Methods: A retrospective study of all DCD cases (n=33) performed at Toronto General Hospital from January 2011 to December 2020 were matched 1:3 with NDD cases (96) for a total of 129 pancreas transplantations. All statistical analysis and graphs were performed using GraphPad Prism 9 software. Continuous data are presented as mean and standard deviations, categorical data as total numbers and percentages and Kaplan Meier method was used to estimate patient and graft survival. A significant P value was set to ≤0.05.
Results: Patient demographic characteristics are presented in Table 1.
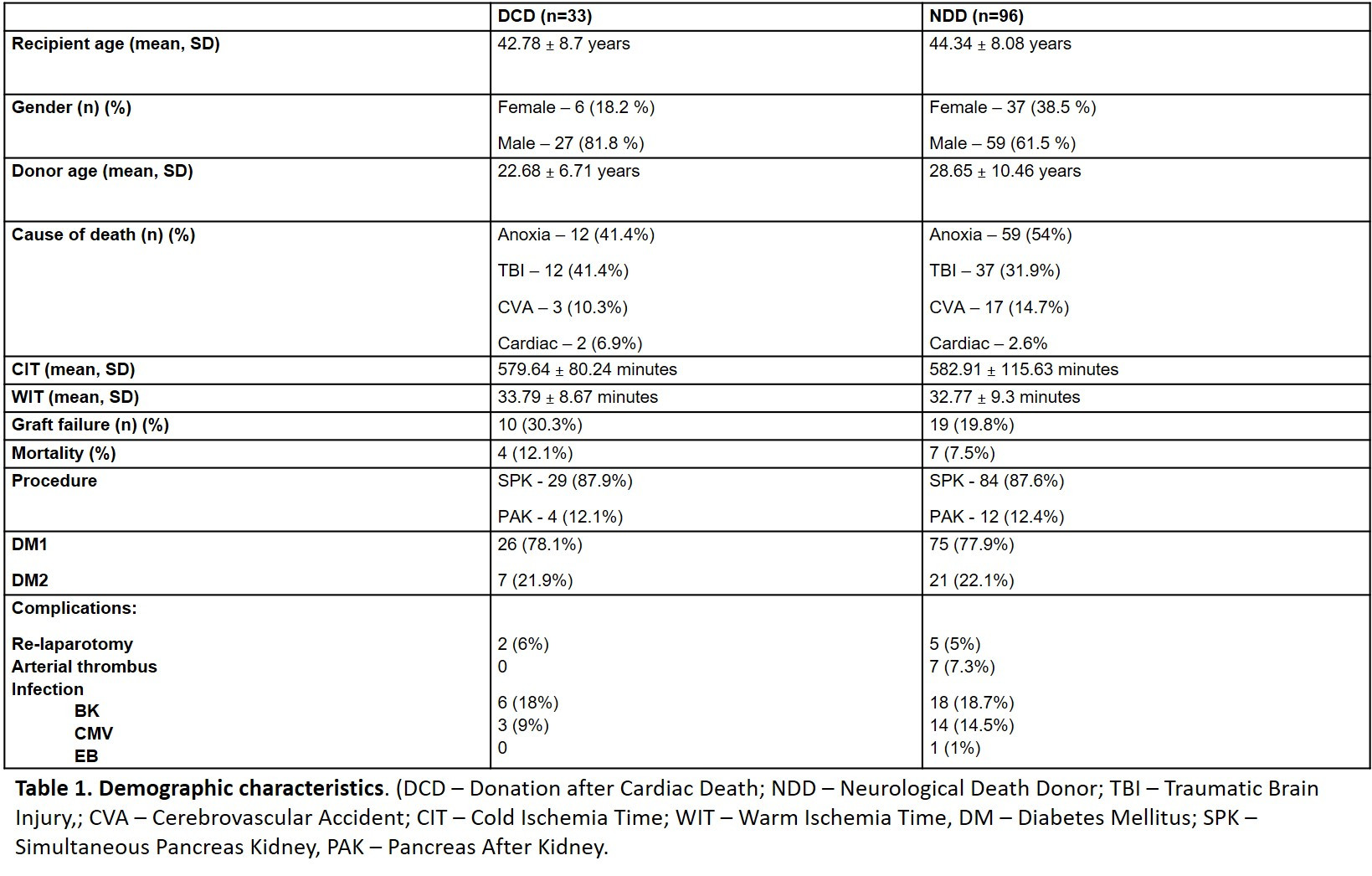
In both groups, the majority of the recipients were male (DCD 81.81% vs NDD 61.45%). Major cause of death was anoxia in both groups and DM1 was the principal diagnosis in pancreas allograft recipients. Simultaneous Pancreas Kidney transplantation was the most common procedure performed (DCD 87.9% vs NDD 87.6%). Graft failure and mortality were comparable between recipients of DCD and DBD grafts (p = 0.21 and p=0.42, respectively). There was no statistically significant difference in graft and patient survival for 1, 5 and 8 years between groups (Figure 1).

Conclusion: Our data suggests there is no difference in outcomes in recipients of grafts from DCD versus DBD donors. The use of DCD grafts is safe and feasible and should be encouraged to become a standard practice to meet the increasing waiting times and number of patients in need of a pancreas allograft.

right-click to download
