
Preventing encephalopathy after isolated small bowel transplantation through portal graft drainage
Emilio Canovai1,2, Irum Amin1,2, Lisa Sharkey1,3, Dunecan Massey1,3, Charlotte Rutter1,3, Jeremy Woodward1,3, Neil Russell1,2, Andrew Butler1,2.
1Cambridge Centre for Intestinal Rehabilitation and Transplant (CamCIRT), Addenbrooke's Hospital, Cambridge, United Kingdom; 2Department of Transplant Surgery, Addenbrooke's Hospital, Cambridge, United Kingdom; 3Department of Gastroenterology, Addenbrooke's Hospital, Cambridge, United Kingdom
Introduction: In isolated small bowel transplantation (SBTx), two methods of drainage have traditionally been described: systemic and portal. Although portal drainage (PD) is more physiological, allowing for the liver ‘first pass effect’, systemic drainage (SD) is often technically more feasible and has been shown in previous studies to have no significant side effects. In this single-centre study, we analyzed our experience over the years with both techniques.
Methods: We performed a retrospective analysis of our prospectively maintained data collected between 2007 and 2022. The following data was included in the study: age, gender, cause of intestinal failure, indication for transplantation, type of portal anastomosis (SD vs PD), infection rate, rejection rate, rate of encephalopathy and patient/graft survival.
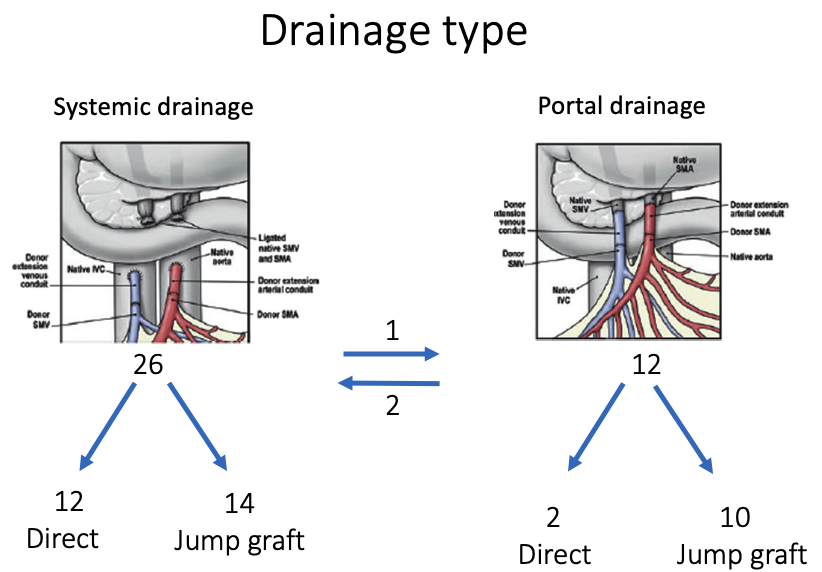
Results: Between October 2007 and March 2022, 38 isolated SBTx were performed in 37 patients (n=15, 41%) males, median age 47 years (21-65)). The most common indication was short bowel (n=32, 86%) with either impending loss of vascular access (n= 10, 27%), IFALD (n=11, 30% or a combination (n = 5, 14%). Twenty-six patient (68%) had SD, while 12 had PD (32%). PD drainage was performed with a venous jump graft in 10 patients and directly in 2.
Postoperatively, there were 12 patients (29%) with either transient or permanent encephalopathy (median ammonia level: 79 μmol/l (42-204)) and 8 patients (24%) with asymptomatic, raised ammonia levels (>30 μmol/l) but without clinical symptoms (38 μmol/l (34-64). All but one patient with clinical encephalopathy had SD. Median ammonia levels double in SD versus PD patients (71 vs 33.5 μmol/l; p=0.0076).
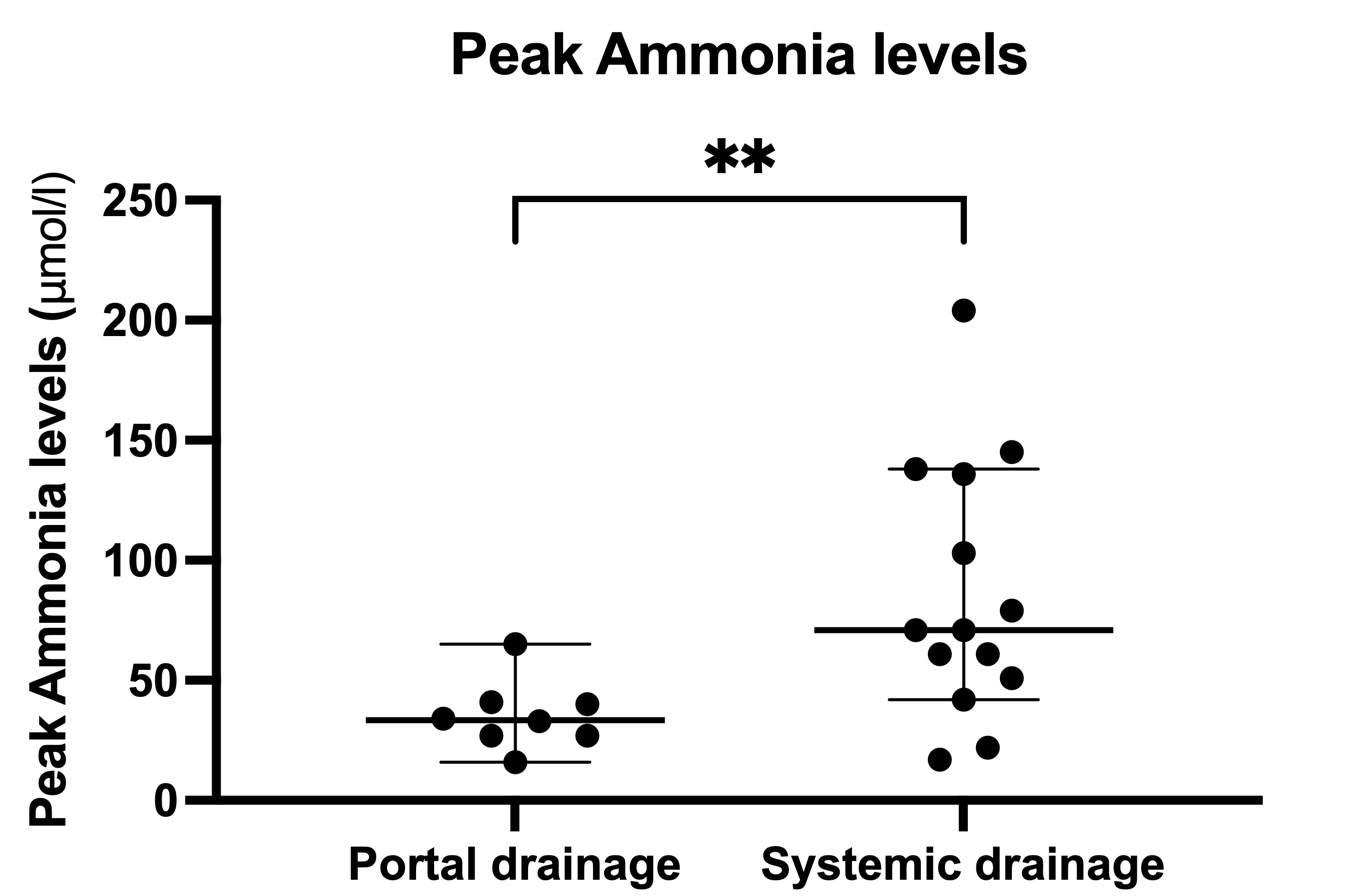
One patient underwent a conversion from a systemic to portal drainage due to severe, intractable encephalopathy using a third-party venous graft. This resulted in a complete reversal of her symptoms and normalization of her ammonia levels from 136 to <10 μmol/l). In three additional patients, conversion from systemic to portal is being considered. Conversely, two patients underwent portal to systemic conversion due to insufficient portal inflow. There were no differences in rates of rejection or patient survival.
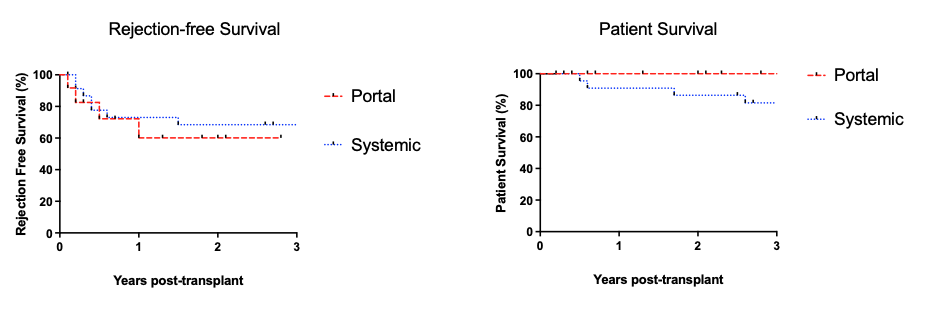
Conclusion: Although, PD and SD yielded equal results in terms rejection and survival rates, encephalopathy was very frequent and occurred only after SD. Given this data, we advocate for PD whenever technically feasible, especially in patient with borderline liver function.

right-click to download
