Antibody-removal therapies in pediatric intestinal and multivisceral recipients: why, when and how? A single-center experience
Maria Lasa1,2, Esther Ramos3, Esther Mancebo1,2, María José Castro-Panete1, Rocío González-Sacristán3, Marta Sarria-Visa3, Ane Miren Andrés-Moreno4,5, Francisco Hernández-Oliveros4,5, Estela Paz-Artal1,2, Paloma Talayero1,2.
1Department of Immunology, University Hospital 12 de Octubre, Madrid, Spain; 2Instituto de Investigación Sanitaria imas12, University Hospital 12 de Octubre, Madrid, Spain; 3Unit of Intestinal Rehabilitation and Transplant, University Hospital La Paz, Madrid, Spain; 4Department of Pediatric Surgery, University Hospital La Paz, Madrid, Spain; 5IdiPaz Research Institute, University Hospital La Paz, Madrid, Spain
Introduction: Donor specific anti-HLA antibodies (DSA) impact negatively on the outcome of intestinal grafts. Although the use of antibody-removal therapies (ART) is becoming more frequent in the last years, issues regarding their timing and effectiveness remain under discussion, especially when they are detected in the absence of any clinical symptom.
Methods: From an initial cohort of 119 transplants, 81 transplants were finally included in the analysis (those without anti-HLA study or in which donor specificity could not be assessed were discarded). ART was performed with different combinations of intravenous immunoglobulin (0,5 g/kg), plasmapheresis and rituximab (boluses of 375 mg/m2 with a maximum of 4 dosis). Anti-HLA antibodies were tested by Luminex assay.
Results: A total of 14 ART procedures were performed in 12 transplants from 10 recipients (Table 1) under the following indications: A) peri-transplant due to preformed DSA (n=3), B) DSA in the context of rejection (n=4), C) dnDSA without rejection (n=5) and D) DSA persistence (n=2).
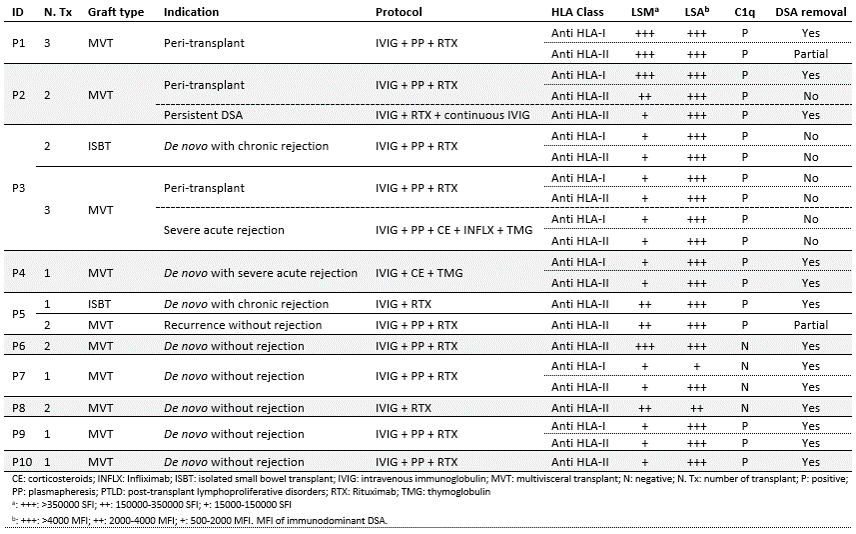
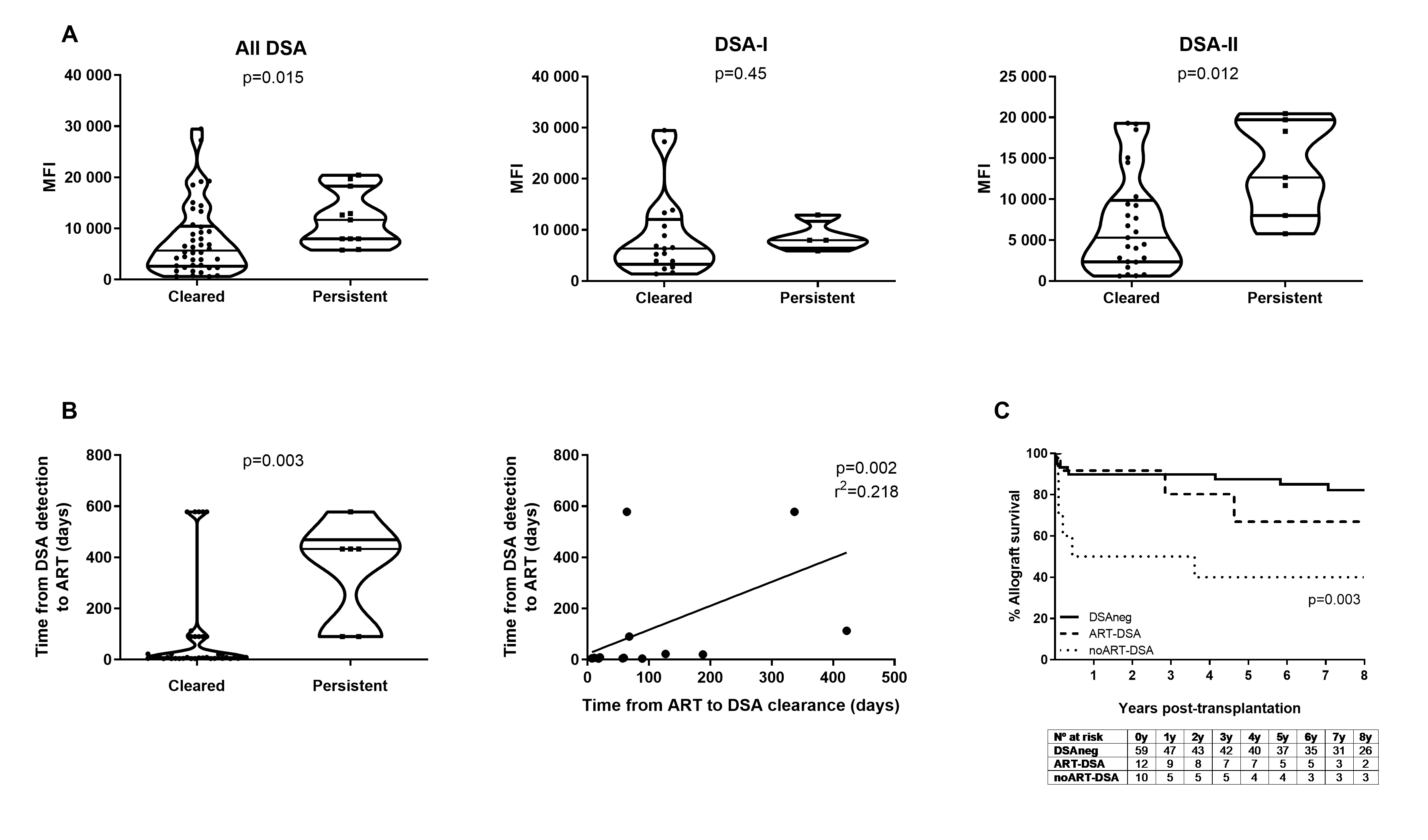
Considering as successful outcomes both the complete DSA removal and the partial decrease (in number of specificities and/or DSA intensity), ART resulted effective in the 79% of the procedures (11/14), 83% of transplants (10/12) and 90% of recipients (9/10). Regarding the indication, ART showed a 100% effectiveness in patients treated for dnDSA without clinical symptoms, whereas it decreased to 67% for preformed DSA and DSA in the context of rejection (needing in some cases more than one procedure to achieve the complete clearance). Analyzing the impact of DSA MFI on the ART outcome, we observed that it was significantly higher in persistent than in cleared DSA (p=0.015) (Figure 1A). This difference was mainly attributed to DSA-II, in which MFI values showed to be much more decisive for DSA removal (p=0.012). Another factor relevant for the therapy success was the time between DSA detection and ART starting, this being significantly lower for cleared DSA (p=0.003) (Figure 1B). The 8-year allograft survival in treated recipients was similar to those without DSA. Nevertheless, non-treated patients with DSA showed a significantly lower graft survival (p=0.003) (Figure 1C).
In the 3 transplants in which dnDSA appeared together with rejection the graft loss was unavoidable even the ART was effective in 2 of them. From the remaining 9 cases, 7 transplants were free of rejection. In another 2 cases rejection happened without compromising graft viability and without DSA increase.
Conclusion: The results confirm the ART effectiveness in terms of DSA removal and allograft survival and encourage their early use even in the absence of clinical symptoms.

right-click to download
