
Cost-effectiveness of using a kidney anastomosis facilitation and cooling device to eliminate second warm ischemia time
Keith S Hansen1, Cynthia Yock2, Jan Pietzsch2.
1Department of Surgery, UCSF, San Francisco, CA, United States; 2Biodesign, Stanford University, Palo Alto, CA, United States
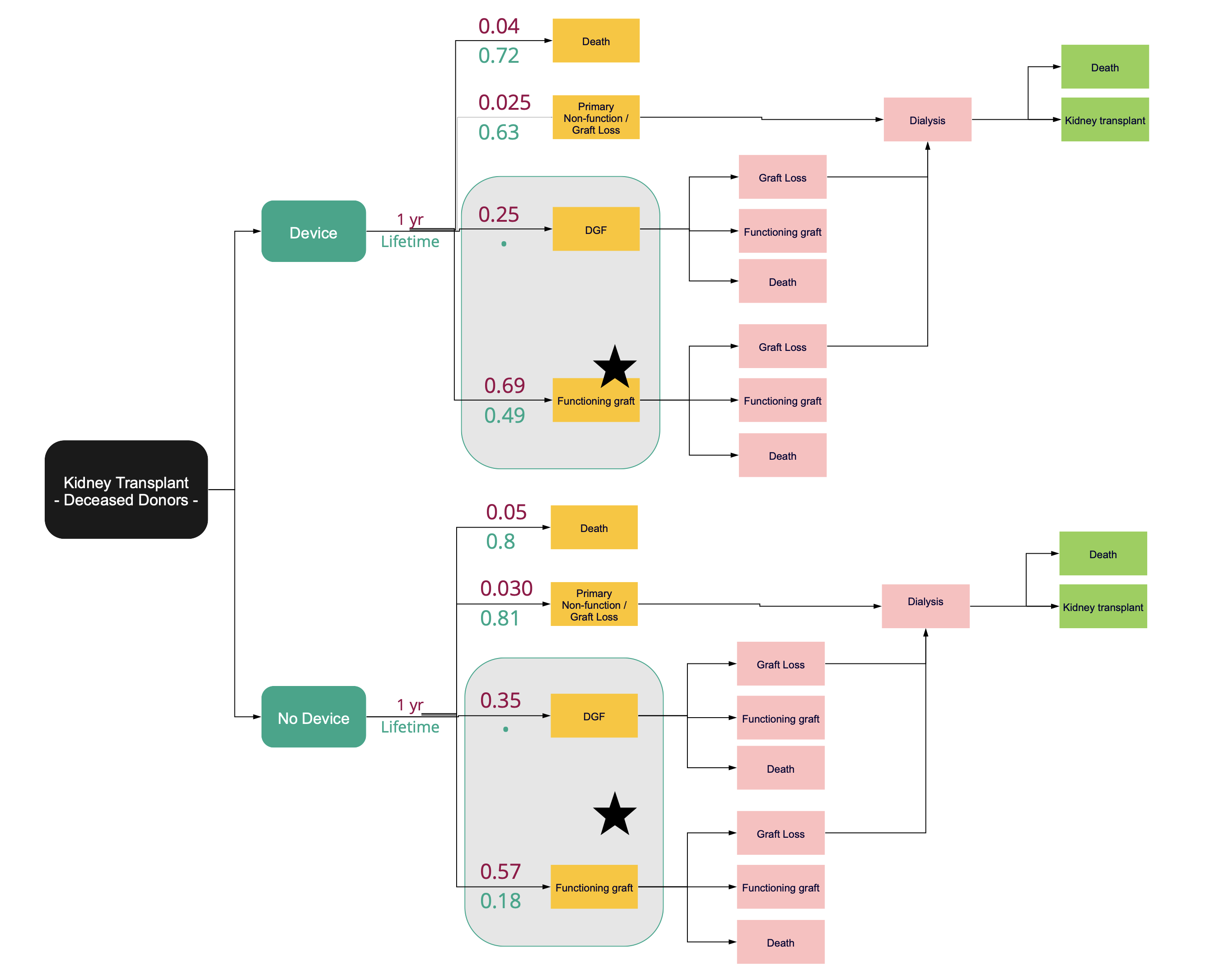
Introduction: The warming of a donor kidney during the vascular anastomosis of a transplant i.e., second warm-ischemia time (SWIT), is independently associated with higher rates of delayed graft function, premature graft failure, and the discard of high-risk kidneys. Existing literature shows that shortened SWIT and intra-operative cooling of a renal allograft during SWIT cumulatively reduces the incidence of delayed graft function in deceased donor kidney transplant recipients from a baseline rate of 35% to 25%, 5-year graft loss from 23% to 16%, and increases the number of transplantable kidneys by reducing the cumulative (first plus second) warm ishcemia time in deceased after circulatory death (DCD) donor kidneys. Cost effectiveness of a breakthrough anastomosis facilitation and SWIT eliminating cooling device was evaluated with a Markov Model.
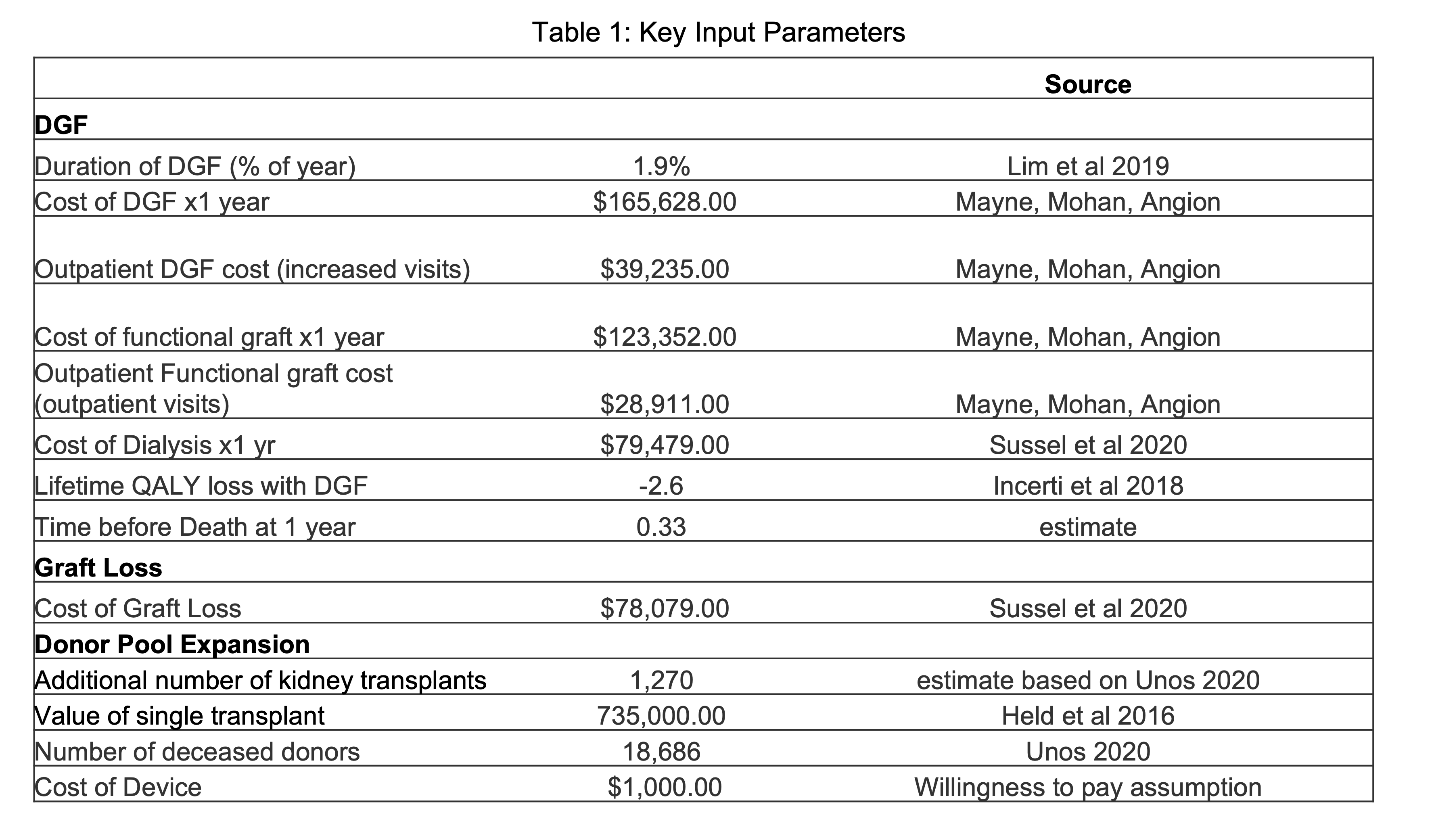
Methods: A state-transition model was used to predict the ff!ect of intra-operative cooling and standard of care on 1-year and lifetime probabilities of having a functioning graft, delayed graft function, graft loss with return to dialysis, and death. We adopted a societal perspective and estimated an incremental-cost-effectiveness ratio in U.S. dollars per quality adjusted life year (QALY).
Results: Intra-operative allograft cooling of deceased donor kidneys provides a 0.01 QALY improvement and $4,800 in savings per patient at 1-year, and over a lifetime, provides 0.26 QALYs and $12,200 in savings per patient. In both the 1-year and lifetime estimates, the ICER is dominant with the cooling device. The total cost savings, not including QALY gains to the system in this group, is $228 million. Including cost savings of the projected increase in organ utilization validated via a surgeon survey (n=175) resulted in $1.18 billion in savings over the lifetime of an annual cohort of transplant recipients. The 95% credible interval for ICER was cost-saving to $39,000 per quality adjusted life year.
Conclusion: The model suggests that intra-operative cooling of a deceased donor renal allograft, over a wide range of assumptions, is a cost effective strategy for transplantation that would result in significant cost savings and lower morbidity and mortality. Use of a breakthrough designated device to eliminate intra-operative warming over a 60 minute period and thereby reduce rates of delayed graft function, increase organ longevity, and change organ acceptance practices would lead to significant cost savings.
Byers Center for Biodesign, Stanford University.

right-click to download
