
Wide spectrum of molecular injury highlights heterogeneity of banff tubulitis and interstitial inflammation lesions
Fuad Shihab1, Daniel Brennan3, Matthew Ellis4, Thin Thin Maw5, Nikhil Agrawal2, Grigory Shekhtman2, Eric Stites6, Jijiao Zeng2, Edmund Huang7, Shiang-Cheng Kung8.
1Medicine, University of Utah, Salt Lake, UT, United States; 2Kidney Transplant, CareDx, Brisbane, CA, United States; 3Medicine, Johns Hopkins University, Baltimore, MD, United States; 4Medicine, Duke University, Durham, NC, United States; 5Medicine, University of Southern California, Los Angeles, CA, United States; 6Medicine, University of Colorado, Aurora, CO, United States; 7Medicine, Cedars Sinai Medical Center, Los Angeles, CA, United States; 8Medicine, University of California, San Francisco, San Francisco, CA, United States
Introduction: The pathological definition and clinical significance of borderline T cell-mediated rejection (BL-TCMR) remains an area of active debate, leading toinconsistencies in therapeutic strategy. Previously published data suggests that donor-derived cell-free DNA (dd-cfDNA) levels at the time of BL-TCMR diagnosismay identify patients at risk of adverse long-term outcomes. We characterized dd-cfDNA levels associated with BL-TCMR among patients enrolled in the Kidneyallograft Outcomes AlloSure Registry (KOAR, NCT03326076).
Methods: Patients with BL-TCMR findings (Banff 2019) on either for-cause or surveillance biopsy and a dd-cfDNA result within 30 days were included in theanalysis. Patients with biopsies showing isolated tubulitis or interstitial inflammation without tubulitis were also analyzed.
Results: We identified 56 cases of BL-TCMR with paired dd-cfDNA results (obtained within 30 days); median dd-cfDNA among these patients was 0.34% (IQR:0.17 - 1.00) (Figure 1a). The differences in dd-cfDNA among individual BL-TCMR combinations (t1/i1, t2/i1, t3/i1, t1/i2, t1/i3) were not significant, though thenumber of t3/i1 (n = 3, dd-cfDNA = 0.04%, 4.85%, 9.06%) and t1/i3 (n = 1, dd-cfDNA = 3.03%) cases was small. No differences were observed between biopsieswith BL-TCMR and those with isolated tubulitis (t1/i0, t2/i0) or isolated inflammation without tubulitis (t0/i1) (Figure 1b). 31 of 56 BL-TCMR cases had prior dd-cfDNA measurement, with median result of 0.24% (IQR: 0.20 - 0.37) obtained 63 (IQR: 53.5 - 100) days before the index biopsy. The median percent increasebetween these sequential results was 55% (IQR: -9 - 235%).
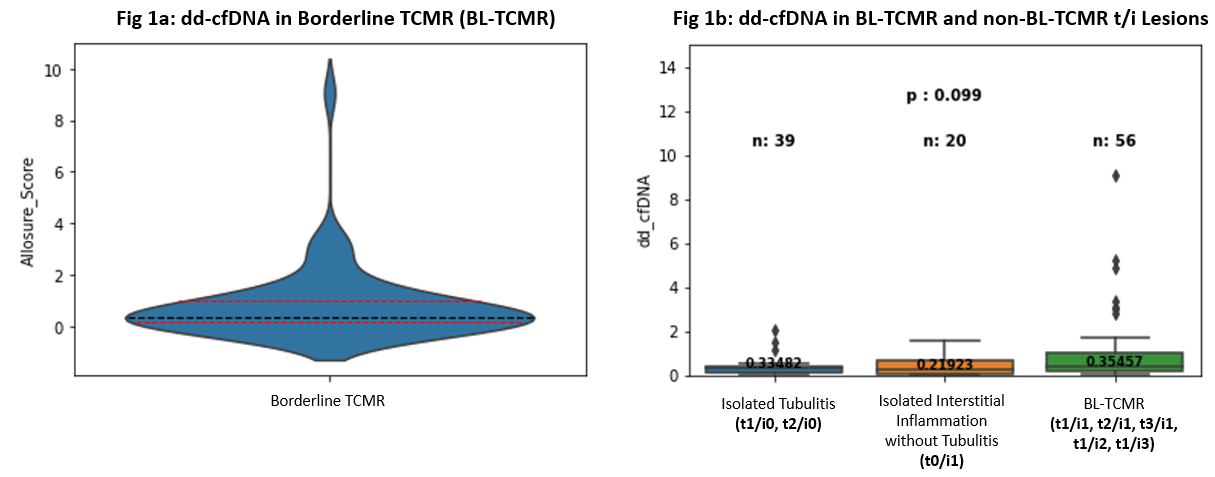
Conclusions: Substantial heterogeneity is observed both with regards to dd-cfDNA levels at the time of BL-TCMR and the trajectory of dd-cfDNA precedingindex biopsy. More importantly, no differences in dd-cfDNA are observed between BL-TCMR and t/i lesions not presently included in Banff criteria for BL-TCMR.These findings suggest that BL-TCMR, isolated tubulitis, and isolated inflammation without tubulitis represent a spectrum of molecular injury that may be further.

right-click to download
