Jiang Liu, People's Republic of China has been granted the TTS International Transplantation Science Mentee-Mentor Awards
PGC1alpha-mediated metabolic reprogramming facilitates M1 macrophage polarization during steatotic allograft dysfunction after liver transplantation
Jiang Liu1,2, Oscar Wai-Ho Yeung2, Li Pang2, Kevin Tak-Pan Ng2, Chung-Mau Lo2, Kwan Man2, Jia-Hong Dong1.
1Hepato-pancreato-biliary Center, Beijing Tsinghua Changgung Hospital, Tsinghua University, Beijing, People's Republic of China; 2Department of Surgery & HKU-Shenzhen Hospital, LKS Faculty of Medicine, The University of Hong Kong, Hong Kong, Hong Kong
Introduction: The pro-inflammatory macrophage activation is the major force to allograft dysfunction, but detailed mechanism is poorly understood. Our previous study demonstrated the pivotal role of PGC1a in mediating steatotic graft injury via mitochondrial regulation (Liu et al., 2020). This study aims to elucidate the role of PGC1a in regulating macrophage polarization regarding metabolic reprogramming during steatotic graft injury.
Method: Intrahepatic PGC1a expression and macrophage subpopulation were quantified and their correlation with acute phase steatotic allograft dysfunction and long-term graft survival was analyzed in a liver transplant cohort. Macrophage subtypes with distinct PGC1a expression patterns were investigated in a rat orthotopic liver transplant model. The functional study of PGC1a in mediating macrophage metabolic reprogramming as well as its polarization were studied in a mouse ischemia and reperfusion model.
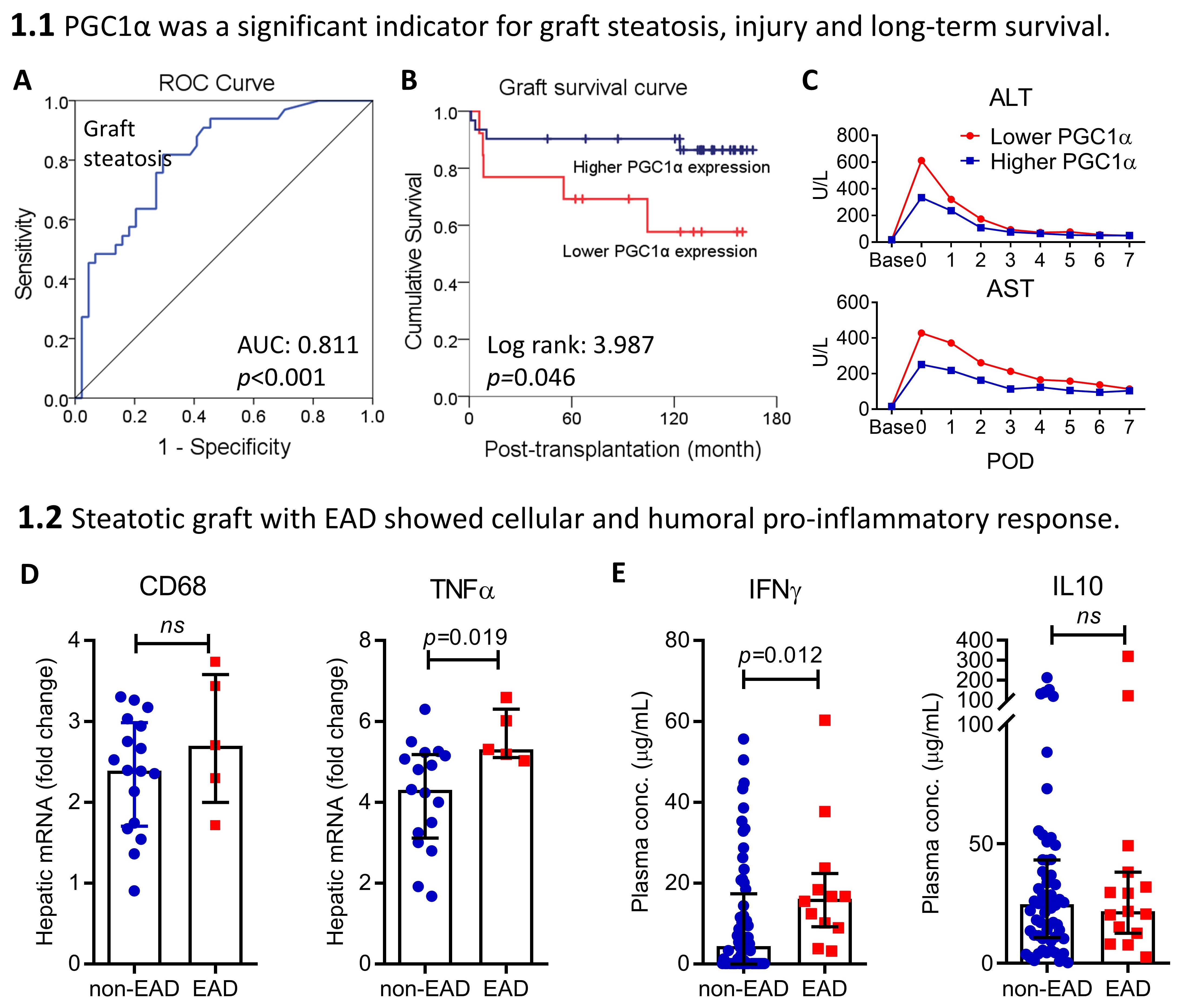
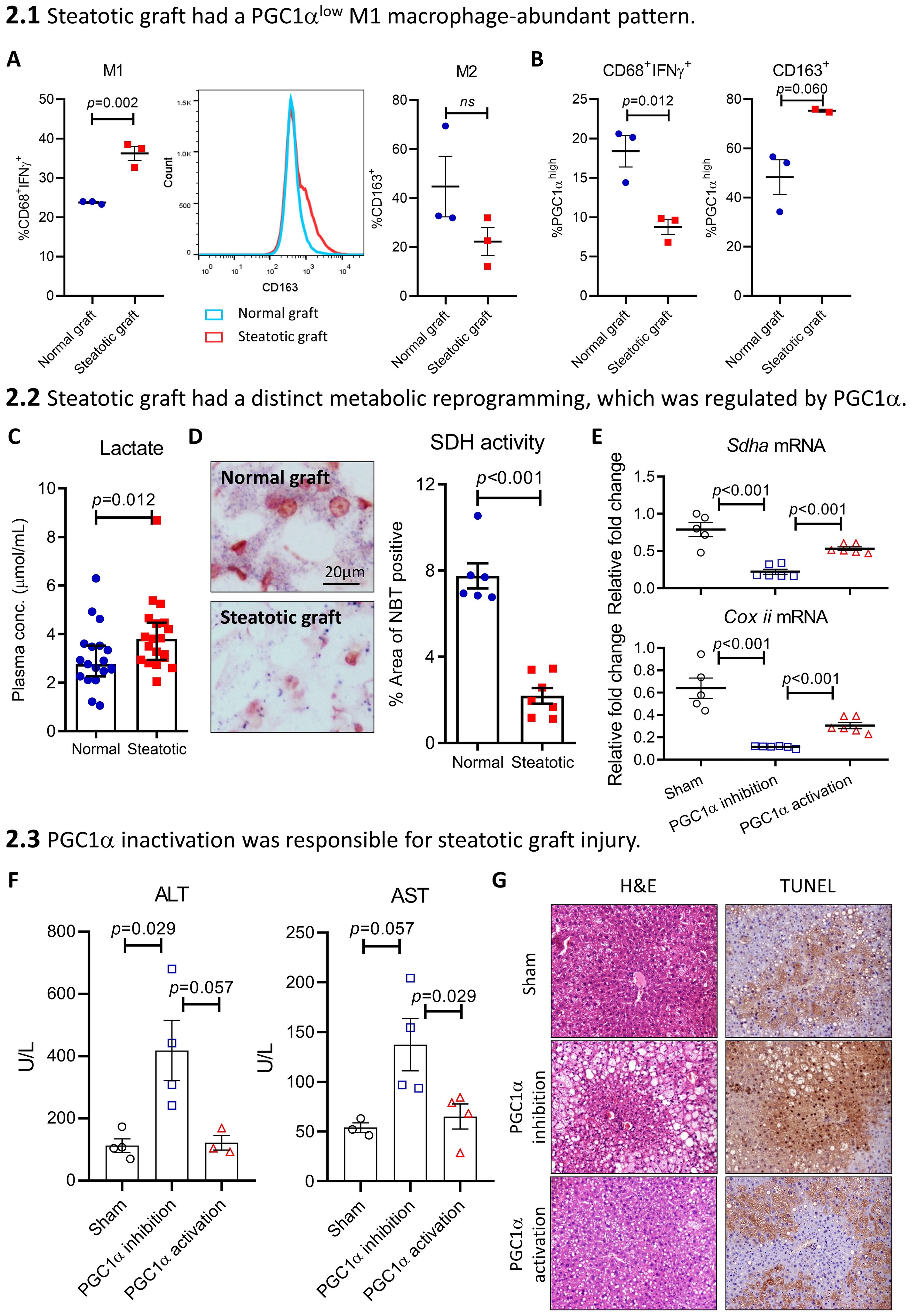
Results: The cutoff value of intrahepatic PPARGC1A (PGC1a) mRNA level (relative fold change=0.385) was determined by the ROC curve with AUC of 0.811 (p<0.001) (Fig. 1A). Divided by PGC1a cutoff, lower expression recipients using steatotic grafts were shown significantly deteriorated long-term graft survival as well as acute phase elevation of ALT and AST (Fig. 1B-1C). The cytokine quantification showed that patients with early allograft dysfunction (EAD) had both cellular and humoral pro-inflammatory response, which were indicated by increased CD68 and TNFa expression in the graft and elevated IFNg but decreased IL10 concentration in the plasma (Fig. 1D-1E). Further consolidated by the rat liver transplant models, steatotic graft had a higher M1 macrophage ratio but lower M2 ratio (Fig. 2A). Especially, the subgroups of CD68+IFNg+PGC1alow macrophage and CD163+PGC1ahigh macrophage were both higher in the steatotic graft compared with the normal graft (Fig. 2B). Detailed metabolism analyses showed that steatotic graft had down-regulated oxidative phosphorylation (OXPHOS) but enhanced glycolysis, which were indicated by increased plasma lactate level and decreased OXPHOS complex II (succinate dehydrogenase, SDH) activity (Fig. 2C-2D). Functional study showed that inhibition of PGC1a decreased the expression of OXPHOS subunits Sdha and Coxii, but reactivation of PGC1a restored their expression (Fig. 2E). Consistently, inhibition of PGC1a in liver showed elevated ALT and AST, exacerbated portal triad inflammation, as well as extended steatosis and apoptosis, whereas reactivation of PGC1a attenuated these phenomena (Fig. 2F-2G).
Conclusion: PGC1a is pivotal in mediating steatotic graft injury via promoting intrahepatic M1 macrophage polarization through metabolic reprogramming.
Reference: Liu J, Pang L, Ng KTP, et al. Compromised AMPK-PGC1alpha Axis Exacerbated Steatotic Graft Injury by Dysregulating Mitochondrial Homeostasis in Living Donor Liver Transplantation. Ann Surg. 2020.

right-click to download
