The role of liver transplant in the management of hepatoblastoma patients
Mingxuan Feng1,2, Tiffany Cho-Lam Wong3, Hongting Huang1,2, Patrick Ho Yu Chung3, Ping Wan1,2, Jianjun Zhu1,2, Yi Luo1,2, Lei Xia1,2, Chung Mau Lo3, Qiang Xia1,2.
1Liver surgery, Renji Hospital, Shanghai Jiaotong University School of Medicine, Shanghai, People's Republic of China; 2Shanghai Institute of Transplantation, Shanghai, People's Republic of China; 3Department of Surgery, Queen Mary Hospital, The University of Hong Kong, Hongkong, Hong Kong
Background: Hepatoblastoma (HB) is a rare malignancy. Liver resection (LR) and liver transplant (LT) are potential curative treatment, but the selection strategy for LT remains unclear. This study aimed to define the selection criteria between LR and LT. Method This was a retrospective study from 2 university centers. All patients with HB who received chemotherapy and surgical treatment from 2014 to 2020 were included. Patients who had unresectable disease after chemotherapy would be offered LT. Salvage LT would be considered if patients developed recurrence after LR. Multivariable analysis was conducted to identify risk factors for inferior event free survival (EFS) after LR and to determine the impact of such risk factors in the LT cohort.
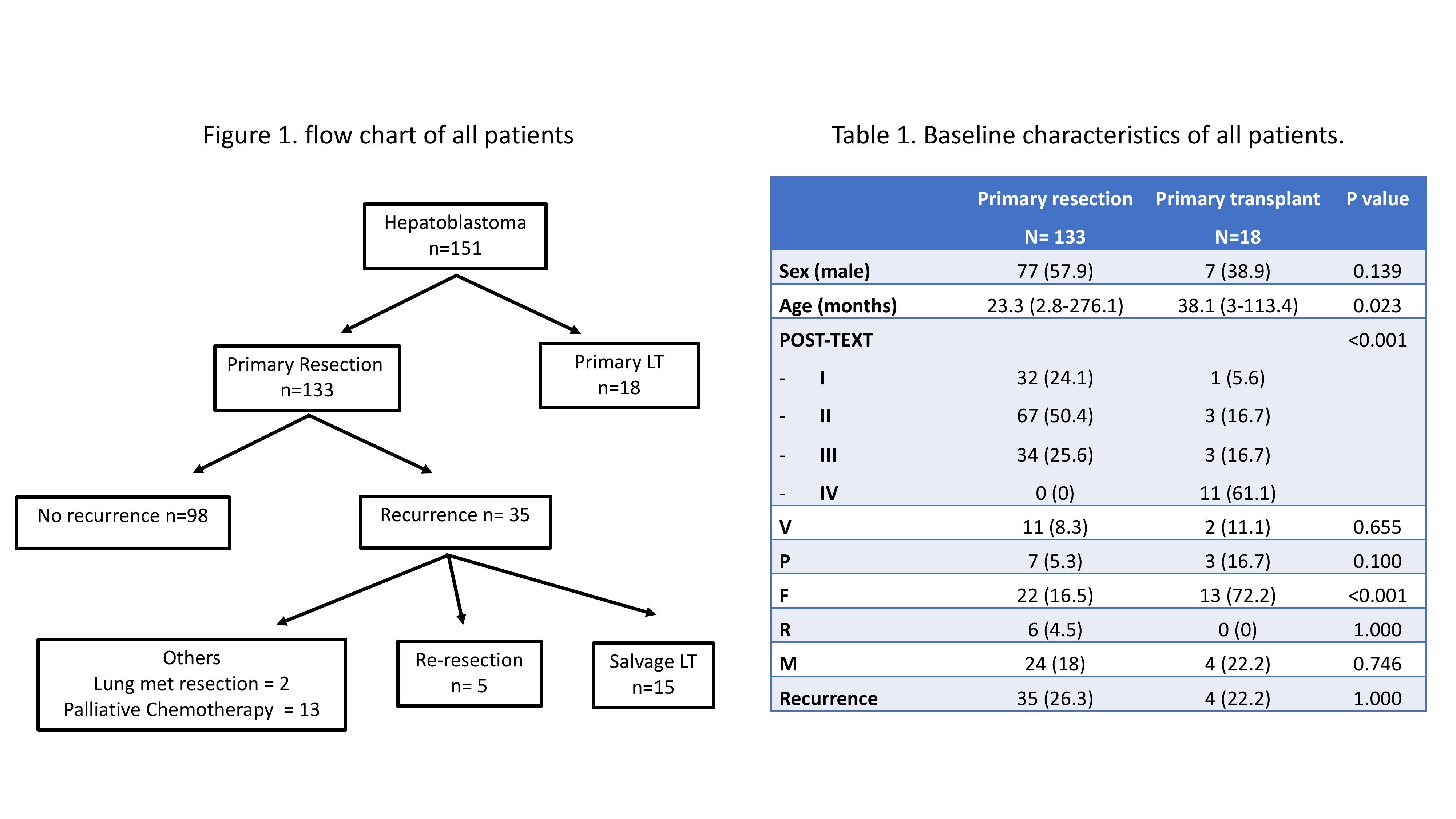
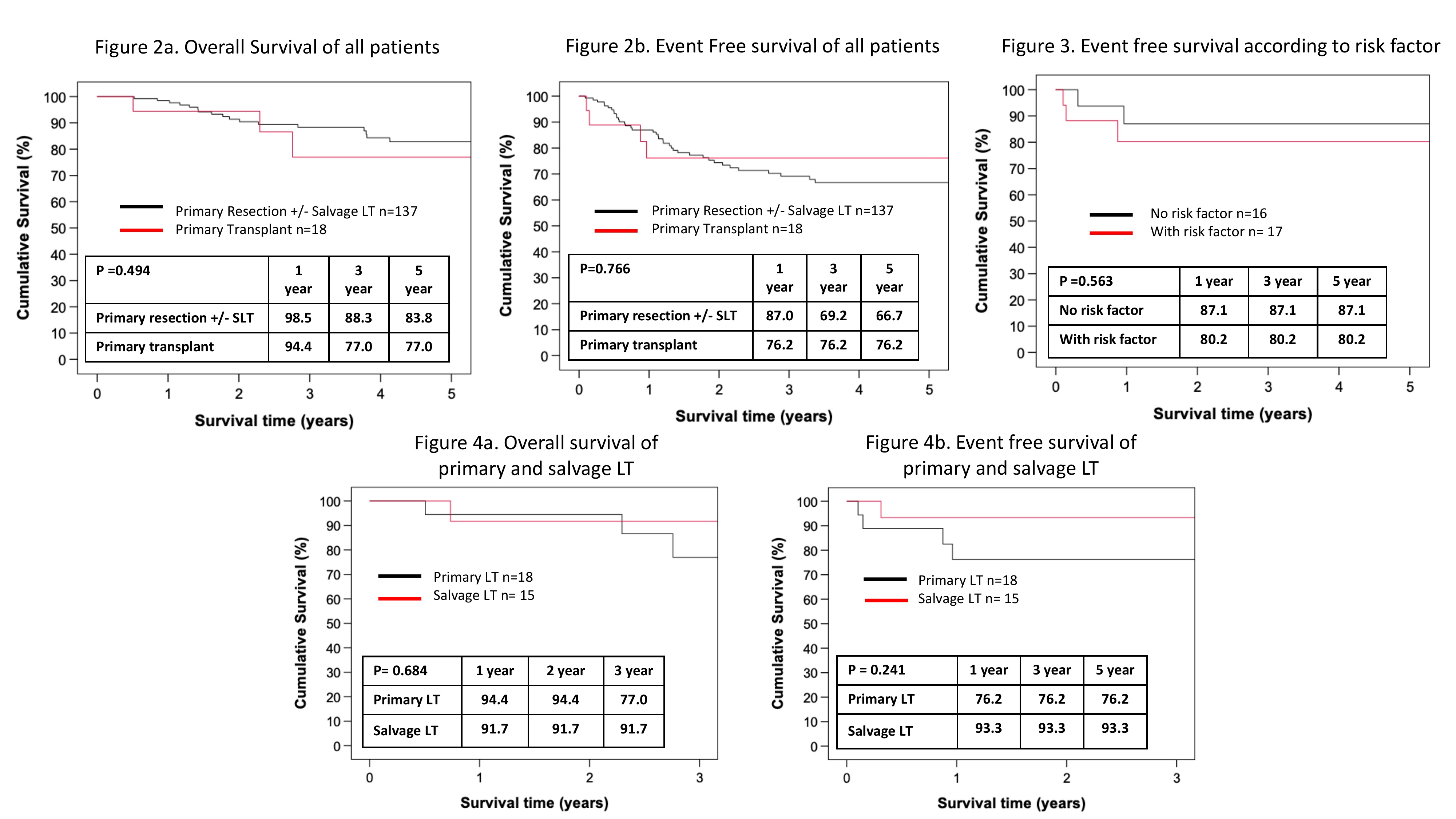
Results: One hundred and fifty-one HB patients were included; 133 (88.1%) patients had primary LR and 18 (11.9%) had primary LT. The flow chart of all study patients was presented in Figure 1. As LT was reserved for patients who had unresectable disease after chemotherapy, the POST-TEXT stage was more advanced in the primary LT group. (Table 1) Nonetheless, the overall survival (OS) and EFS were similar between primary LR and primary LT group. Figure 2a and 2b. In multivariable analysis among the LR group, 2 risk factors were associated with poor EFS: multifocality HR 3.294 95% CI (1.739-6.243), P <0.001 and rupture HR 3.772 95% CI (1.321-10.777), P=0.013. The LT group were stratified into 2 groups based on the presence of risk factors. The 5-year EFS after LT was 87.1% and 80.2%, in the absence and presence of risk factor respectively. (Figure 3) Fifteen patients underwent salvage LT and their outcomes were compared to patients who underwent primary LT. The OS and EFS were comparable. (Figure 4a and 4b).
Conclusion: HB patients who had multifocal disease and rupture were associated with inferior EFS and LT should be considered. The outcomes of salvage LT were comparable to primary LT and it should be offered as a curative treatment in patients with recurrent HB.

right-click to download
