Outcomes of duct-to-duct biliary anastomosis in pediatric liver transplantation using left sided graft
Mingxuan Feng1,2, Ping Wan1,2, Yi Luo1,2, Jianjun Zhu1,2, Lei Xia1,2, Qiang Xia1,2.
1Liver Surgery, Renji Hospital, Shanghai Jiaotong University School of Medicine, Shanghai, People's Republic of China; 2Liver Surgery, Shanghai Institute of Transplantation, Shanghai, People's Republic of China
Background: Roux-en-Y hepaticojejunostomy(HJ) is the standard-of-care for biliary reconstruction in pediatric liver transplantation(LT), especially in left sided grafts. This study aimed to investigate the learning curve and the risk of biliary complication of duct-to-duct biliary anastomosis(DDA) in pediatric LT using left sided grafts.
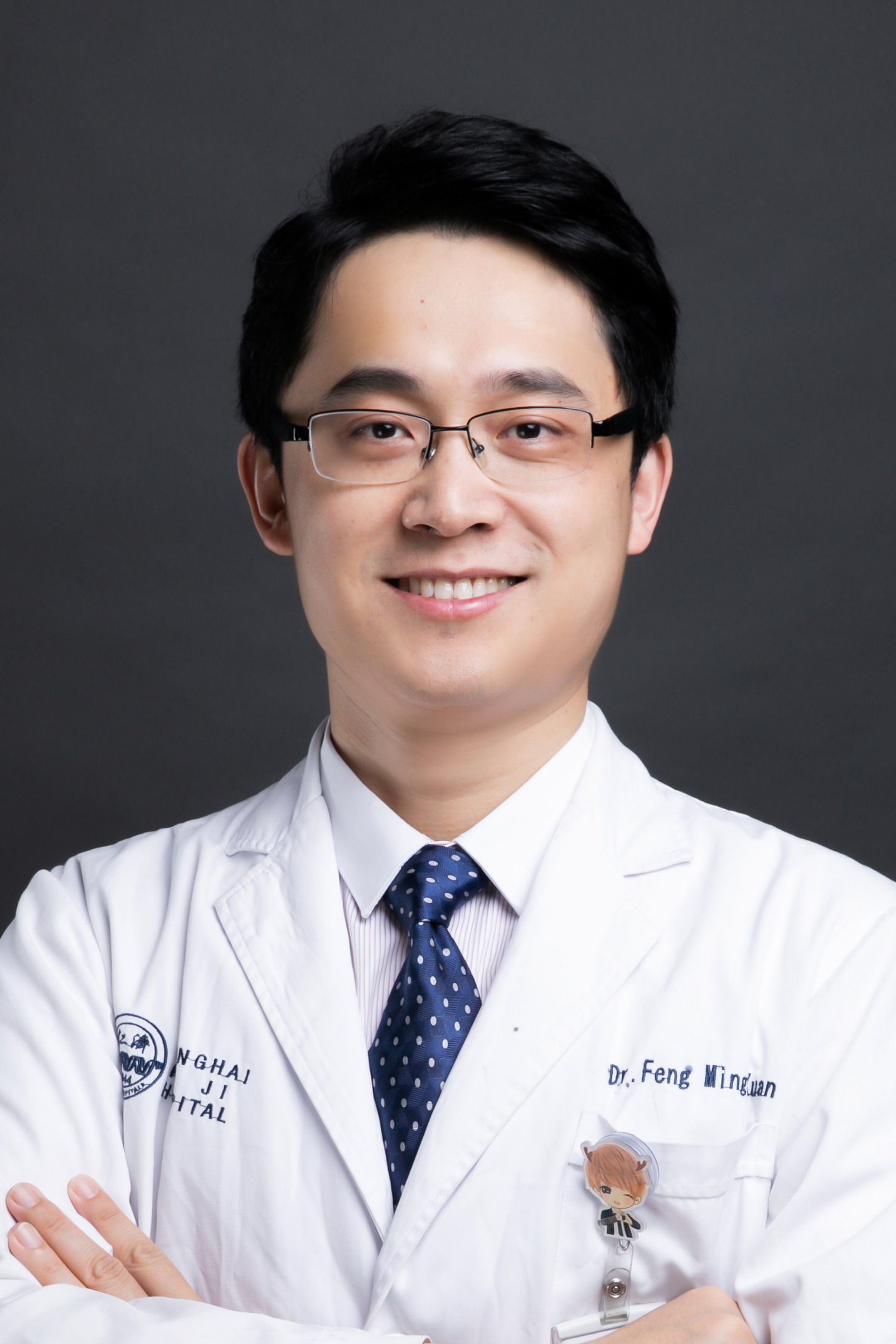
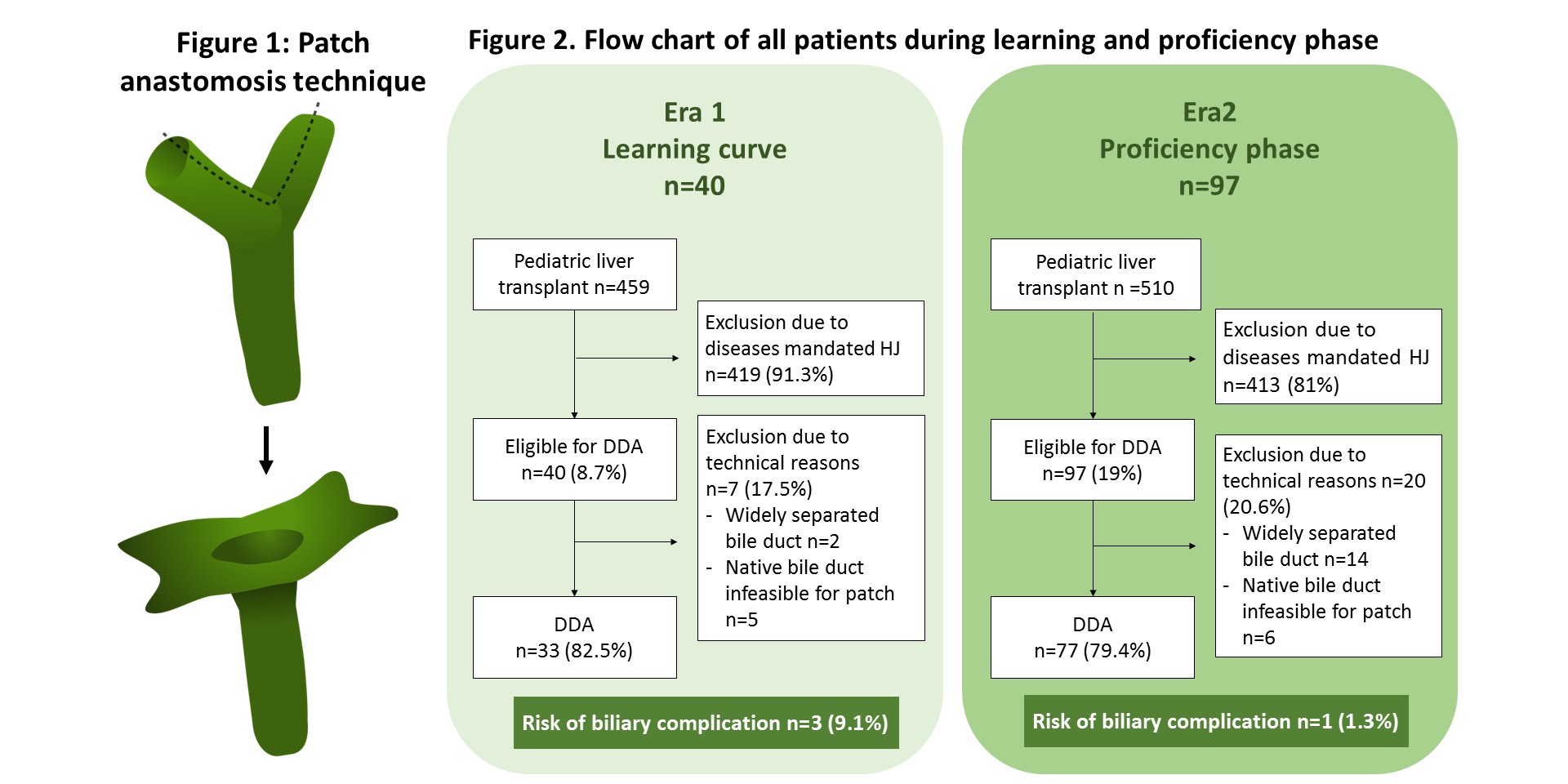
Method: This was a retrospective study from a surgical unit of a university-affiliated center. From 2017-2020, DDA was performed in pediatric LT with a high hilar dissection and patch anastomosis technique under a prospective protocol.(Figure 1) The exclusion criteria were: 1) disease mandated HJ, 2) widely separated graft bile ducts that ductoplasty was infeasible, 3) native biliary anatomical factors that rendered a patch infeasible. Size discrepancy was not a contraindication. The primary endpoint was the risk of biliary complication at 1-year after LT.
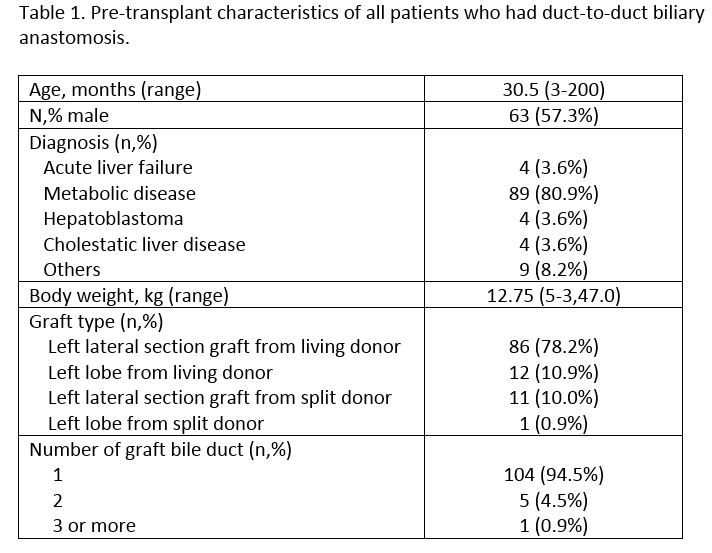
Results: During study period, 137 pediatric recipients fulfilled inclusion and were considered eligible for DDA, 110 (80.3%) patients had DDA. The pre-transplant characteristics were listed in table 1. The first 40 patients belonged to learning curve period and after that, more patients were eligible for DDA (7.2% vs. 15.1%, P<0.001). The overall risk of biliary complication at 1-year was 2.9% (4/137) and it was higher in the learning phase (9.1% vs 1.3%, P=0.045). Of the 4 biliary complications: 1 had bile leakage and stricture and required endoscopic stenting; 3 had biliary stricture with 2 required conversion to HJ and 1 had endoscopic stenting. All 4 patients have normal graft function at time of analysis. There was only one hospital mortality (1/137, 0.7%) and was due to post-operative bleeding and was unrelated to biliary complication. Graft survival rates at 1-and 3-year after DDA were 98.2% and 96.8% respectively.
Conclusion: DDA was safe and feasible with excellent perioperative and long-term outcomes and should be considered the primary choice for biliary reconstruction in eligible pediatric transplant patients.

right-click to download
