
Preoperative neutrophil and platelet-to-lymphocyte ratio as predictors of mortality and surgical related complications after liver transplantation
Rodrigo Gasque1, Magalí Chahdi1, Marcelo Lenz1, Emilio G. Quiñonez1, Francisco J. Mattera1.
1HPB and liver transplant unit, Hospital de Alta Complejidad "El Cruce", Florencio Varela, Argentina
Introduction: Liver transplantation (LT) is considered the only definitive treatment in patients with end-stage liver disease (ESLD). Nowadays, the 5-year overall survival (OS) after LT is 75%–85%. In addition, short-term mortality has decreased due to better perioperative care, advancements in operative techniques, as well as changes in patient selection. Despite these improvements, a subset of patients still dies within the first year after LT. Neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) have been recently reported as simple and useful markers of various inflammatory changes and are calculated based on complete blood count data. It has been suggested that both parameters in the acute phase of LT are prognostic factors for early post-transplant survival.
Method: We conducted a retrospective and analytic study. Among 410 LT recipients between January 2013 and February 2022 who were operated at the HPB surgery and liver transplant department of the Hospital de Alta Complejidad “El Cruce”, we selected 120 patients after simple random sampling. Patients’ demographic data, cirrhosis etiology, model for end-stage liver disease (MELD) scores, and hematological parameters were analyzed. Latest hematological parameters prior to surgery were recorded. NLR and PLR values were calculated based on the measured hematological parameters. Time and incidence of postoperative complications were analyzed. Fisher exact test, Mann–Whitney U test and Students T-test were used when appropriate. Two-sided p value equal or less than 0.05 was considered to indicate statistical significance with a confidence interval of 95%. All analyses were conducted using MedCalc version 20.027 (https://www.medcalc.org/).
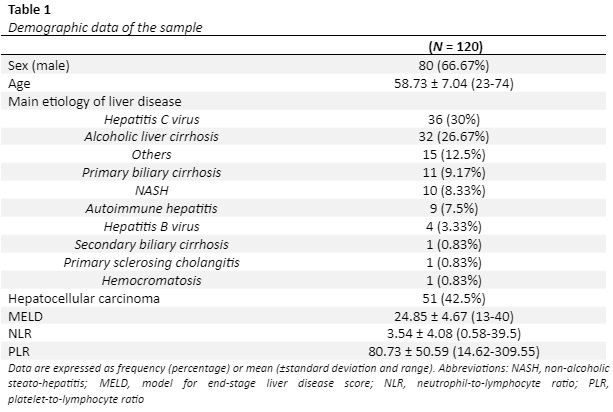
Results: The mean age of the 120 patients included in the study was 58.73 ± 7.04 years; 66.67% were male. All patients received decesead donor liver transplantation. The most common indication for LT was liver cirrhosis due to hepatitis C virus (HCV) (30%) followed by alcoholic liver cirrhosis (26.67%) (table 1). The mean MELD score was found to be 24.85 ± 4.67. 23 out of 120 patients died after LT (19.16%). 5 patients (4.16%) presented surgical-related complications. Mortality was higher in patients with higher MELD scores (p = 0.011). The mean preoperative NLR was 3.54 ± 4.08 and PLR was 80.73 ± 50.59. When NLR and PLR results with cut-off values of >3,77 and ≤34,18 respectively were compared with the incidence of major complications (Dindo-Clavien ≥3) a significant result was found (p = 0.01). No statistical significance was found between NLR, PLR and age and mortality (p=0.91, 0.93 and 0.47 respectively).
Conclusion: Preoperative NLR and PLR were not found useful to predict mortality after OLT in our series. However, they may be of value to anticipate poor prognosis or major incidence of complications in patients undergoing OLT. With this simple indices, high-risk patients can be identified and preventive measures can be taken.

right-click to download
