An analysis of deceased donor liver offers to adolescent compared to young adult liver transplant candidates
David Cron1,2, Rafal Mazur3, Joel Adler2,4, Heidi Yeh1.
1Surgery, Massachusetts General Hospital, Boston, MA, United States; 2Center for Surgery and Public Health, Brigham and Women's Hospital, Boston, MA, United States; 3Harvard Medical School, Boston, MA, United States; 4Surgery and Perioperative Care, Dell Medical School, University of Texas at Austin, Austin, TX, United States
Introduction: Minimizing waitlist mortality among pediatric liver transplant candidates is a priority. Yet, organ acceptance practices are variable, and half of the children who die on the waitlist receive at least one liver offer that is declined. It is unclear if the willingness to accept liver offers differs between adolescent and young adult candidates. We studied deceased donor liver offer acceptance in adolescent vs. young adult liver transplant candidates, hypothesizing that adolescents would have lower acceptance rates than young adults.
Methods: This was a retrospective cohort study using the SRTR registry and potential transplant recipient file to identify deceased donor liver offers to liver transplant candidates aged 11-26 between 2009-2019. We excluded the following offers: those refused due to size, offers to candidates outside of the first 40 positions on the waiting list, and offers for livers that were ultimately discarded. We additionally stratified the analysis by quality of offered liver, defining lower quality as donation after circulatory death donors, steatotic livers (≥30% macrosteatosis), or donors >40 years old. Our exposure was candidate age: adolescent (11-17yo) vs. young adult (18-26yo). The outcomes compared across age groups included: number of offers received, liver offer acceptance, transplant rate, waitlist mortality, and removal for being too sick. We compared these offer metrics for higher vs. lower quality donor liver offers. Offer acceptance rate was adjusted for MELD/PELD at listing, donor age, and donor/candidate size.
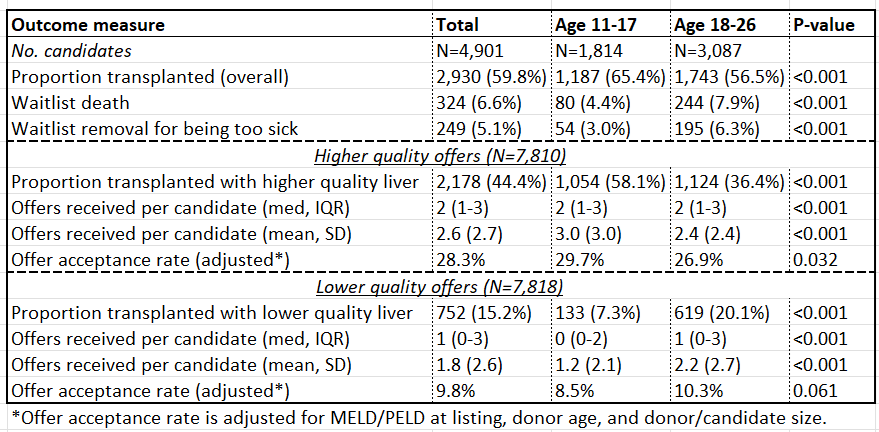
Results: We studied 15,628 liver offers (50% higher quality) to 4,901 waitlisted candidates (37% age 11-17, 63% 18-26). The table shows offer metrics by age group. Compared to young adults, adolescents were more likely to be transplanted (65.4% vs. 56.5%, P<0.001) and less likely to die (4.4% vs. 7.9%, P<0.001) or be removed from the waitlist (3.0% vs. 6.3%, P<0.001). Adolescent recipients were less likely than young adults to receive a lower quality liver (11.2% vs. 35.5% of recipients, P<0.001). The overall acceptance rate for higher quality liver offers was 28.3%. Adolescents received more high-quality offers (3.0 vs. 2.4, P<0.001) and had slightly higher acceptance of these offers (29.7% vs. 26.9%, P=0.032) compared to young adults. For lower quality offers, adolescents received fewer offers (1.2 vs. 2.2, P<0.001) and had a similarly low acceptance rate (8.5 vs. 10.3%, P=0.061).
Conclusion: Seven out of ten transplantable deceased donor liver offers received by pediatric and young adult candidates are declined on their behalf. Offer acceptance rates for high quality livers are similarly low for adolescents and young adults. Efforts to increase offer acceptance rates, taking care to safeguard post-transplant outcomes, may improve access to pediatric liver transplantation.
Research reported in this abstract was supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under Award Number F32DK128981. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.

right-click to download
