Patient experience of the kidney transplant waitlist: an Australian cohort study
Nicole De La Mata1, Victor Khou1, Juliet Byrnes1, Patrick J Kelly1, James Hedley1, Rachael Morton2, Angela C Webster1,2.
1Sydney School of Public Health, Faculty of Medicine and Health, The University of Sydney, Camperdown, Australia; 2NHMRC Clinical Trials Centre, The University of Sydney, Camperdown, Australia
Introduction: People on the kidney waitlist are counselled on expected waiting time, but are less informed about their waitlist experience, including temporary or permanent removal from waitlist (i.e. delisted). Disparities may exist in who is delisted. We aimed to describe and evaluate factors associated with the patient journey after entering the waitlist for deceased donor kidney transplant regardless of whether they were transplanted or not.
Method: We included all incident patients waitlisted for their first kidney transplant from deceased donor in Australia between 1st Jul 2006 and 31st Dec 2019. We described all clinical transitions after entering the kidney waitlist including: active on waitlist; delisted; kidney transplant; graft failure; death and censored (Fig 1). We summarized the median time to each transition until first transplant and annual percentages in each clinical state until 5 years. We used multi-state Markov model to evaluate factors associated with transitions after entering the waitlist until first transplant, reporting the hazard ratio (HR) for each transition.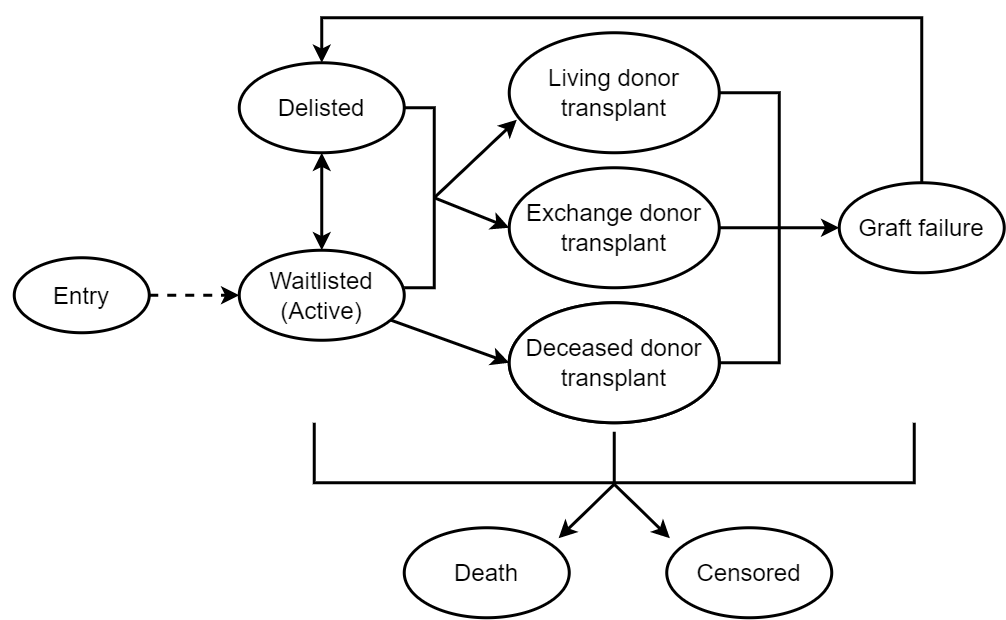
Results: 8,466 people entered the kidney waitlist where 6,741 people received their first transplant (6,163 deceased donor; 506 living donor; 99 paired kidney exchange donor), 381 people died while waiting (31 active on waitlist; 350 delisted) and 1,344 were still waiting for a transplant (844 active on waitlist; 500 delisted) by the end of follow-up. Nearly two-thirds (63%) were never delisted while waiting, but 2,111(25%) were delisted once and 1,016(12%) were delisted ≥2 times. Of those delisted, 47% spent a total of <6 months off-waitlist. Median time from waitlist to transplant increased with number of times delisted, from 4.8 months (IQR:1.7 months-1.2 years) in patients never delisted to 3.2 years (IQR:2.1-4.6 years) in patients delisted ≥2 times. At 1-year, the probability of transplant was 41%(95%CI:40-42%), active on waitlist was 42%(95%CI:41-43%), delisted was 11%(95%CI:10-12%) and death was 1.4% (95%CI:1.2-1.7%) (Fig 2). At 5-years, this increased to 63% (95%CI:62-64%) transplanted, 5% (95%CI:4-5%) active on waitlist, 10% (95%CI:9-11%) delisted and 13% (95%CI:12-14%) died.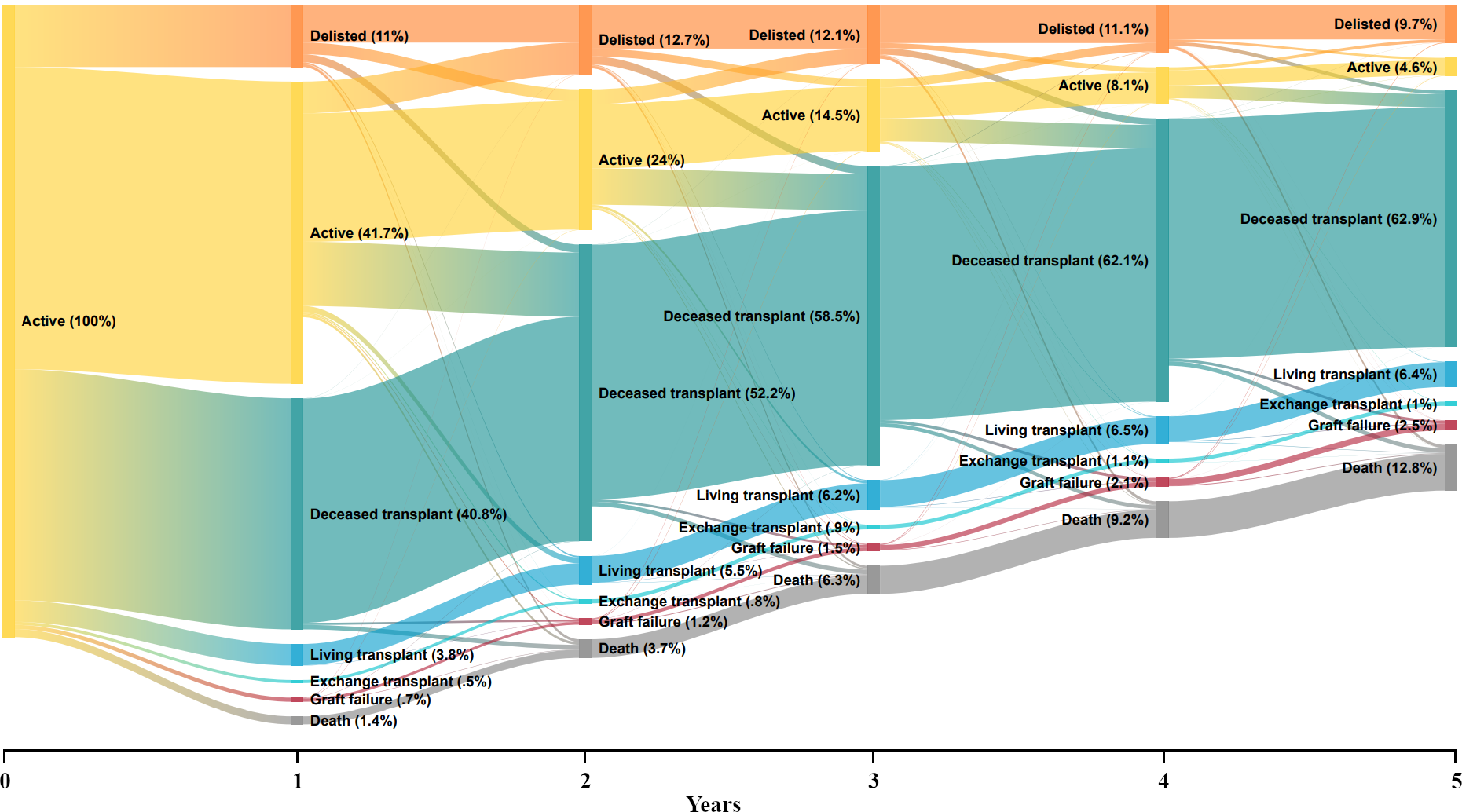
Factors associated with increased likeliness of transitioning from active to delisted included age at waitlist entry (≤29 years: 1.21HR, 95%CI:1.09-1.35; ≥65 years: 1.15HR, 95%CI:1.04-1.27), more recent year of commencing dialysis (2016-19: 1.34HR, 95%CI:1.22-1.47), AB blood group (1.26HR, 95%CI:1.02-1.55), delisted more than once (1.63HR, 95%CI:1.52-1.75), number of comorbidities (one: 1.24HR, 95%CI:1.16-1.33) and cause of kidney failure (diabetes: 1.38HR, 95%CI:1.26-1.50).
Conclusion: The patient experience on transplant waiting list was not straightforward, where about one-third of patients were delisted at least once and had longer time to transplant. Our findings will aid in counselling patients and further support in younger patients may benefit their return to waitlist.

right-click to download
