
The risk of venous thromboembolism is enhanced after a cytomegalovirus infection in kidney transplant recipient
Christophe Masset1,2, Anne Scemla3, Clarisse Kerleau1, Celine Bressolette2, Florent Le borgne4, Emmanuel Morelon5, Fanny Buron5, Moglie Lequintrec-Donnette6, Vincent Perrin6, Marc Ladrière7, Sophie Girerd7, Christophe Legendre3, Alexandre Loupy3, Antoine Sicard8, Laetitia Albano8, Carmen Lefaucheur9, Denis Glotz9, Christophe Mariat10, Guillaume Claisse10, Jacques Dantal1,2, Magali Giral1,2.
1Institut de Transplantation Urologie Néphrologie (ITUN), Centre Hospitalo-Universitaire de Nantes, Nantes, France; 2Center for Research in Transplantation and Translational Immunology, INSERM UMR 1064, Université de Nantes, Nantes, France; 3Service de Néphrologie - Transplantation rénale Adulte, Hôpital Necker-Enfants Malades, Assistance Publique-Hôpitaux de Paris, Paris, France; 4INSERM UMR 1246 - SPHERE, Université de Nantes, Nantes, France; 5Service de Transplantation, Néphrologie et Immunologie Clinique, Hospices Civils de Lyon, Hôpital Edouard Herriot, Lyon, France; 6Department of Nephrology and Renal Transplantation, Lapeyronnie Hospital , Montpellier, France; 7Renal Transplantation Department, Brabois University Hospital, Nancy, France; 8Nephrology, Dialysis and Transplantation Department, Pasteur 2 Hospital, Nice University Hospital, Nice, France; 9Department of Nephrology and Kidney Transplantation, Saint-Louis Hospital, Assistance Publique-Hôpitaux de Paris, Paris, France; 10Service de Néphrologie, Dialyse et Transplantation Rénale, Hôpital Nord, CHU de Saint-Etienne, Saint Etienne, France
DIVAT Consortium.
Introduction: In immunocompetent patients, past CMV infections have been associated with an increased risk of venous thromboembolism (VTE). In this study, we have investigated in a large prospective cohort of kidney transplanted recipients (KTR) whether the occurrence of a CMV infection which is the most frequent pathogen encountered within the first-year post transplantation could be followed by an increased risk of VTE in addition to the risk of the post-operative period, or repeated hospitalizations.
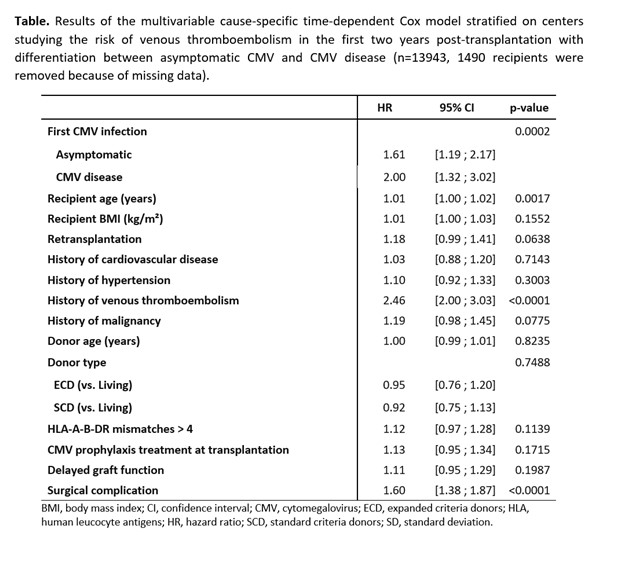
Methods: We conducted a study on the multicentric DIVAT database which was carried out prospectively and exhaustively on key dates during post-operative follow-up of clinical and biological data for all incident KTR belonging to 8 French transplantation centers (CNIL decision DR-2015-087, N°914184). Multivariable cause-specific time-varying Cox models stratified on centers were used to estimate the relationship between the risk of VTE occurring after well documented first CMV infections (asymptomatic or disease) and which were considered as a time-dependent variable.
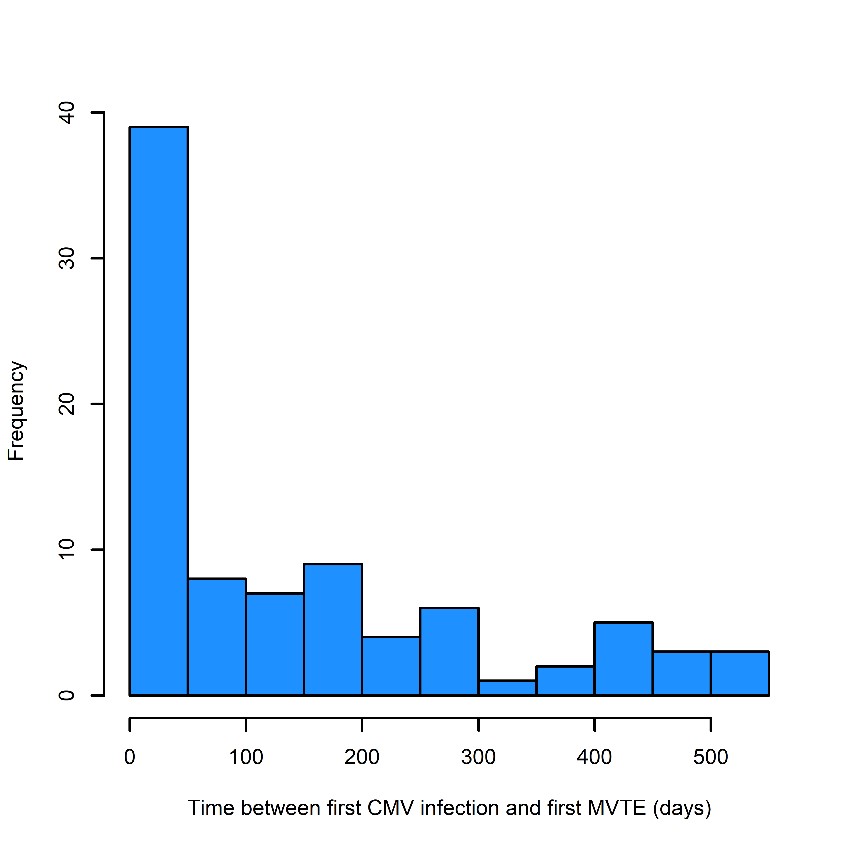
Results: 15433 KTR transplanted between 2000 and 2021 were included among whom 1756 presented a CMV infection with a cumulative incidence at 1- and 2 years respectively of 11.6% [95% CI from 11.1% to 12.2%] and 13% [95% CI from 12.4% to 13.5%]). Within the same period of survey VTE occurred in 5.53% (95% CI from 5.17% to 5.92%) and 6.71% (95% CI from 6.31% to 7.14%) at 1- and 2 years respectively. CMV and VTE was observed in 87 KTR. The final multivariable cause-specific time-varying Cox model stratified on centers showed that after a first asymptomatic CMV infection (n=1176) the risk of VTE is 1.61 [95%CI 1.19; 2.17]. The risk enhanced at 2.00 [95%CI 1.32 ; 3.02] after a symptomatic infection (n=574) in comparison to similar patients free of CMV infection and independently of recipient age, past history of TVE and post-transplant surgical complications. Finally, the increased risk of VTE occurrence did not change whatever it was a primo or a reactivation of the CMV.
Conclusion: After CMV infections and particularly in case of CMV disease, there is an increased risk of VTE. Since to the high frequency of CMV infection after a kidney transplantation, transplant physicians should be aware of such association for a rapid diagnosis and adapted treatment.
The authors would like to thank all patients who participated in this study and the medical and nurse teems who took and take care of them. We also thank the clinical research associates who participated in the data collection and analyses. *DIVAT (Données Informatisées et VAlidées en Transplantation) Consortium, DIVAT Cohort Collaborators (Medical Doctors, Surgeons, HLA Biologists): Lyon Lionel Badet, Antonin Bouchet, Fanny Buron, Sameh Daoud, Valérie Dubois, François Gaillard, Arnaud Grégoire, Alice Koenig, Charlène Lévi, Louis Manière, Xavier Matillon, Emmanuel Morelon, Maud Rabeyrin, Thomas Rimmelé, Olivier Thaunat; Montpellier: Nicolas Abdo, Sylvie Delmas, Moglie Le Quintrec, Vincent Pernin, Hélène Perrochia, Jean-Emmanuel Serre, Ilan Szwarc; Nancy: Alice Aarnink, Asma Alla, Pascal Eschwege, Luc Frimat, Sophie Girerd, Jacques Hubert, Raphaël Kormann, Marc Ladriere, François Lagrange, Emmanuelle Laurain, Pierre Lecoanet, Jean-Louis Lemelle; Anthony Mannuguerra, Charles Mazeaud, Michael Peres; Nantes: Gilles Blancho, Julien Branchereau, Diego Cantarovich, Agnès Chapelet, Jacques Dantal, Clément Deltombe, Lucile Figueres, Raphael Gaisne, Claire Garandeau, Magali Giral, Caroline Gourraud-Vercel, Maryvonne Hourmant, Georges Karam, Clarisse Kerleau, Delphine Kervella, Christophe Masset, Aurélie Meurette, Simon Ville, Christine Kandell, Anne Moreau, Karine Renaudin, Florent Delbos, Alexandre Walencik, Anne Devis; Nice: Laetitia Albano, Fatimaezzahra Karimi, Antoine Sicard, Thierry Wine; Paris-Necker: Lucile Amrouche, Dany Anglicheau, Olivier Aubert, Lynda Bererhi, Christophe Legendre, Alexandre Loupy, Frank Martinez, Arnaud Méjean, Rébecca Sberro-Soussan, Anne Scemla, Marc-Olivier Timsit, Julien Zuber; Paris-Saint-Louis: Denis Glotz, Carmen Lefaucheur. Saint Etienne: Christophe Mariat, Guillaume Claisse.

right-click to download
