A systematic review of perioperative outcomes in robotic assisted kidney transplantation
Arshad Khan1, Hoonbae Jeon2, Alishba Khan3.
1Surgery, Sanford Health, Thief River Falls, MN, United States; 2Surgery, Tulane University, New Orleans, LA, United States; 3Education, Red River High School, Grand Forks, ND, United States
Background: With the advent and accessibility of robotics in surgery in general, RAKT(Robotic-assisted kidney transplantation) is increasingly offered to patients with ESRD. However, the overall advantages over conventional kidney transplants are still debatable. Therefore, this meta-analysis was undertaken to assess the difference in the perioperative outcomes of RAKT versus open Kidney transplantation (OKT).
Methods: Database search was performed following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement to identify studies on the effect of RAKT on surgery duration, kidney failure risk, operative blood loss, length of hospital stay, intraoperative complications, and postoperative complications. The snowball procedure was also used to extract relevant articles from the citations of some included studies. Finally, the Meta-analysis was performed, a random-effects method was applied, and the standard mean difference was used to compute the p-value and I2 value.
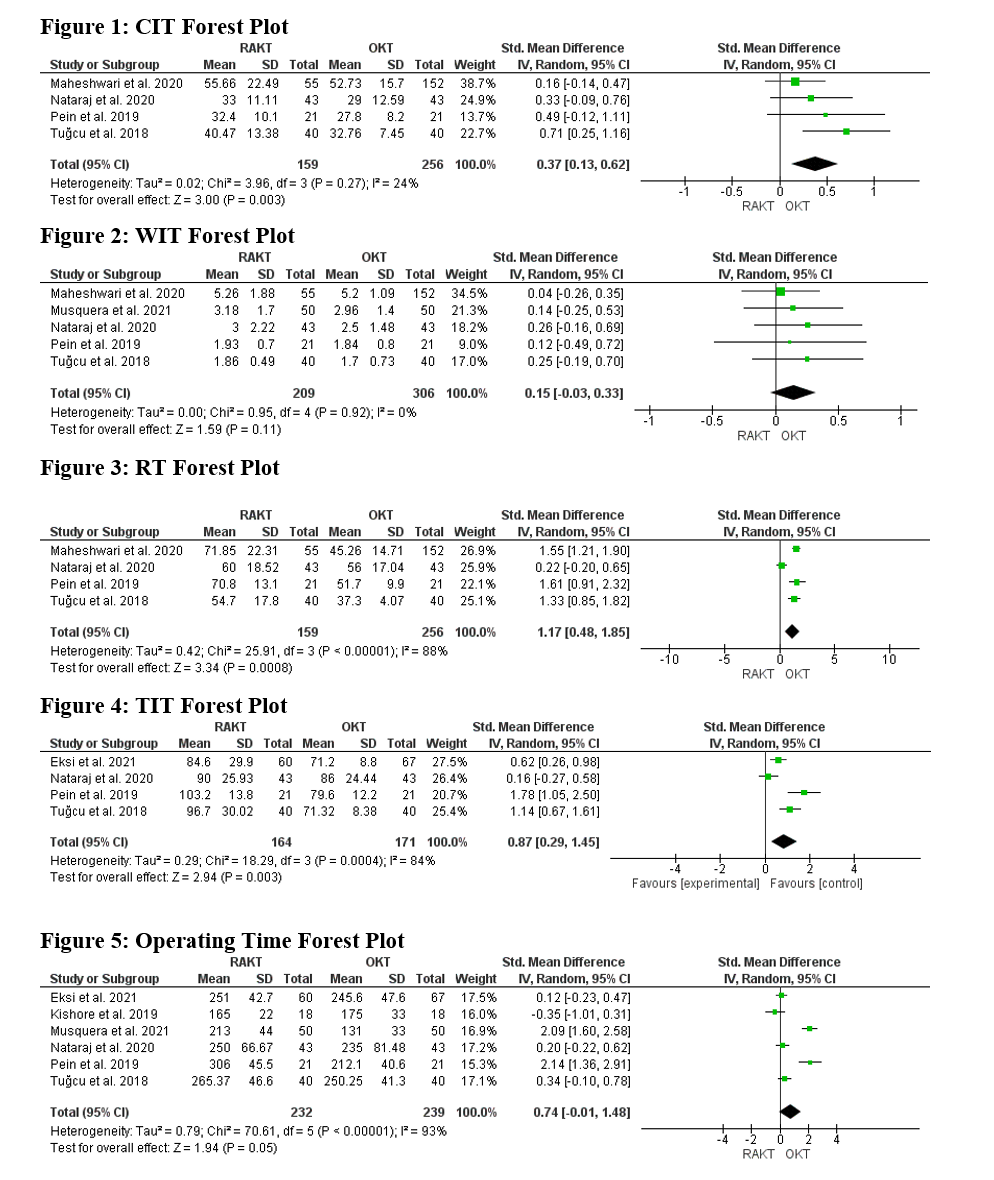
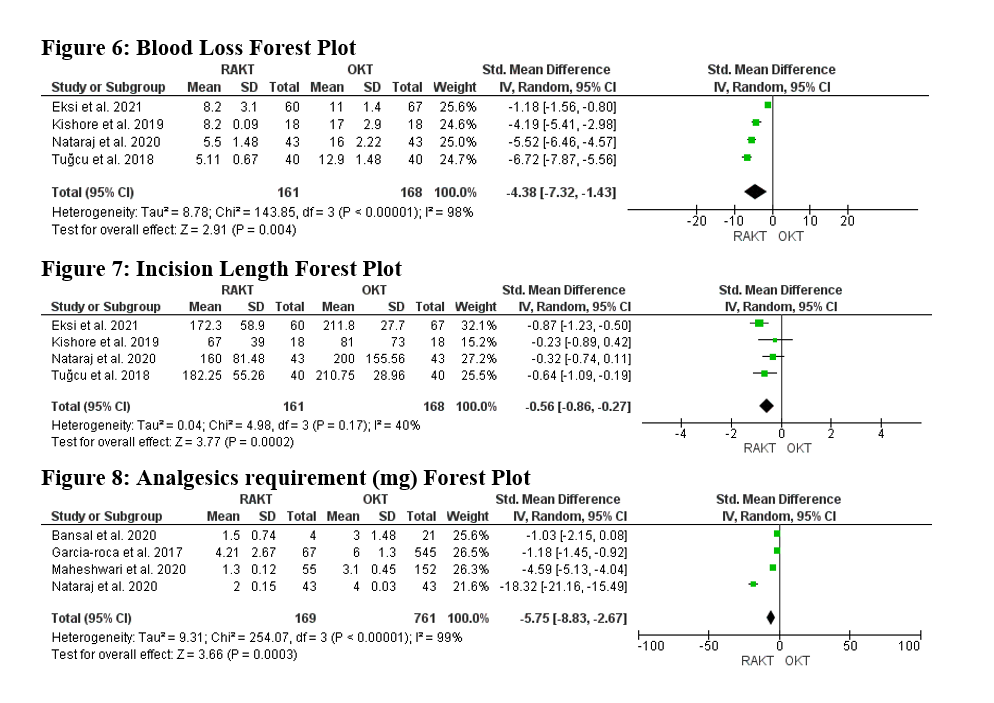
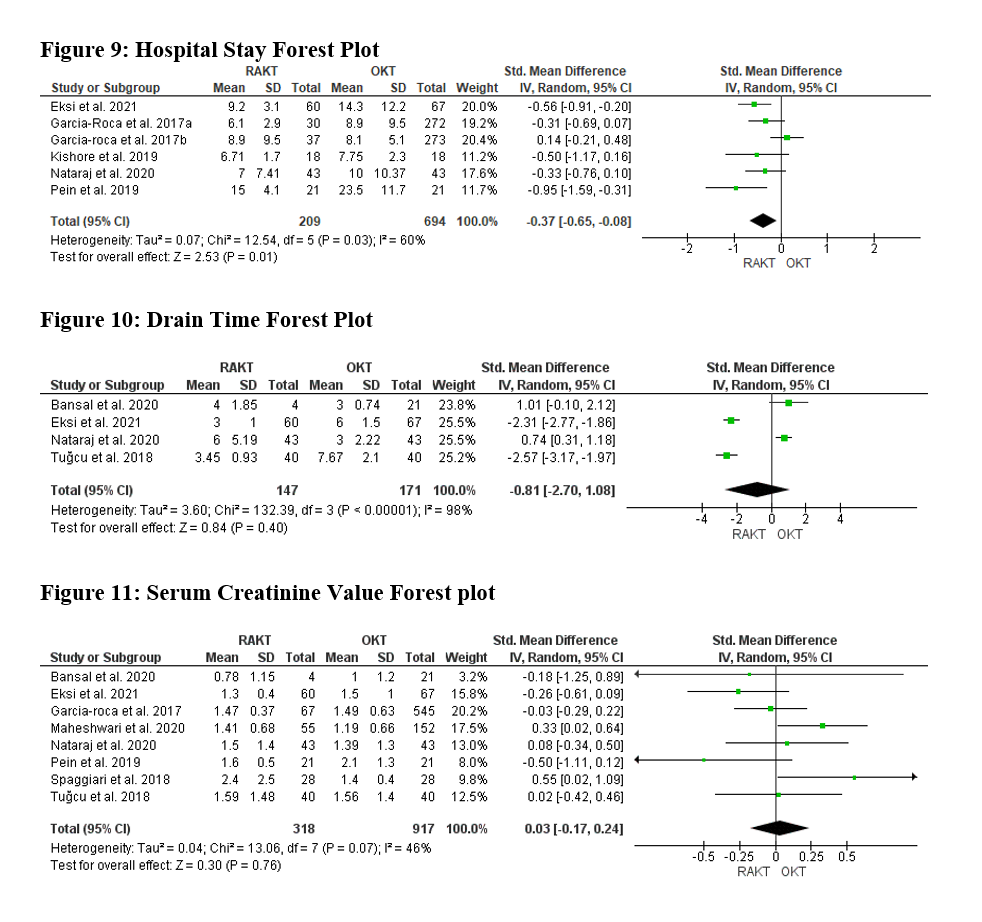
Results: 10 studies yielding 248 patients in the RAKT group and 750 patients in the OKT group were retained for analysis from 327 articles published between 2014 and 2021 that were generated from the database search and another snowballing. The differences in the functional outcomes were not significant across most studies. Of the intraoperative outcomes, pooled results revealed the warm ischemia time (WIT) (SMD = 0.15 [.03, .33], P= 0.11) and operating time (ORT) (SMD = 0.74[-0.01, 1.48], P=0.05) had no significant difference in the RAKT and OKT. The pooled rewarming time (RT), and total ischemia time (TIT) were, however, significantly higher in the RAKT compared to OKT, SMD=1.17[0.48, 1.85], P=0.0008 and SMD=0.87[0.29, 1.45], P=0.003 respectively, but there was no difference in pooled CIT SMD=0.37[0.13, 0.62], P=0.27. The blood loss, incision length and analgesics requirement were significantly lower in the RAKT condition compared to the OKT group at SMD=-0.56[-0.86,-0.27], P=0.0002, SMD=-4.38[-7.32, -1.43], P=0.004, and SMD=-5.75[-8.83, -2.67], P=0.0003 respectively. There was no significant difference for the evaluated postoperative outcome of drain time, and serum creatinine value, SMD=-0.81[-2.73,1.08], P=0.4, and SMD=0.03[-0.17,0.24],P=0.76 respectively, whereas the length of hospital stay and wound infections was smaller for RAKT SMD=-0.37 [-0.65,0.08], P=0.01, and OR 0.20 [0.06-0.62], P=0.006 respectively as shown in figures 1,2 and 3.
Conclusion: RAKT is a safe and feasible alternative to OKT with the advantages of less postoperative pain, a smaller length of incision, fewer wound infections, and a shorter length of hospital stay with equivalent renal graft function and patient outcomes.
Many thanks to Alishba for retrieving the data.

right-click to download
