Long-term outcomes following HLA-incompatible living donor kidney transplantation
Jennifer Motter1, Allan B Massie2, Dorry L Segev2.
1Surgery, Johns Hopkins University, Baltimore, MD, United States; 2Surgery, New York University, New York, NY, United States
Introduction: Incompatible living donor kidney transplantation (ILDKT) offers a survival benefit compared to dialysis for patients with donor specific antibody (DSA) who do not have a compatible living donor. Longer-term outcomes have not been characterized in this population, but must be quantified to inform treatment selection for patients with an incompatible willing donor, and counseling for ILDKT recipients.
Method: We compared 1,406 ILDKT to 17,542 compatible LDKT (CLDKT) recipients using a 25-center cohort from the United States 1997-2016, linked to national registry data (SRTR). Participating centers classified ILDKT recipients as positive Luminex, negative flow crossmatch (PLNF, n=376); positive flow, negative cytotoxic crossmatch (PFNC, n=687); or positive cytotoxic crossmatch (PCC, n=343). We used multivariable Cox regression to quantify the risk of mortality and death-censored graft failure (DCGF), and multilevel mixed-effects linear regression to evaluate eGFR decline (CKD-EPI creatinine equation 2021) in ILDKT and CLDKT recipients.
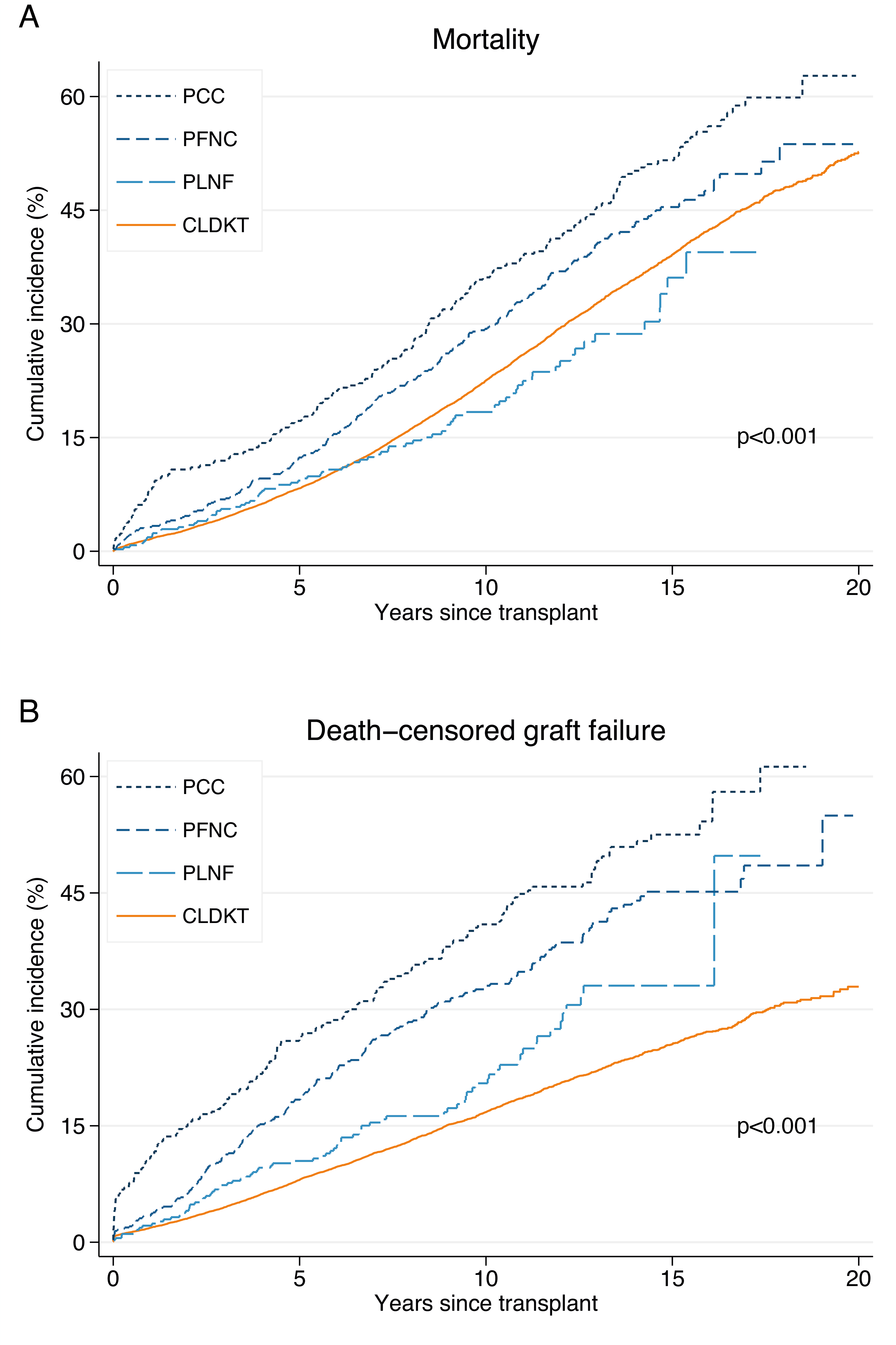
Results: The cumulative mortality risk for CLDKT, PLNF, PFNC, and PCC was: 1.6%, 1.9%, 3.2%, and 8.2% at one year; 22.5%, 18.4%, 29.4%, and 36.1% at ten years; and 39.1%, 36.1%, 45.4% and 51.6% at fifteen-years (p<0.001) (Figure 1A). Although this translated to an equivalent mortality risk for PLNF recipients (aHR=0.830.961.12, p=0.6) after adjustment, PFNC and PCC recipients had a 1.48-fold (aHR=1.301.481.68, p<0.001) and 1.66-fold (aHR=1.331.662.08, p<0.001) higher risk compared their CLDKT counterparts, respectively. The cumulative risk of DCGF for CLDKT, PLNF, PFNC, and PCC was: 1.9%, 2.1%, 3.4%, and 11.1% at one year; 16.8%, 20.5%, 33.1%, and 41.0% at ten years; and 25.5%, 33.1%, 45.2% and 52.5% at fifteen-years (p<0.001) (Figure 1B). After adjustment, this translated to higher DCGF across all levels of DSA strength (aHR PLNF=1.141.411.73, PFNC=1.491.711.95, PCC=1.612.082.67; p for all≤0.001). Conversely, ILDKT and CLDKT recipients had comparable average eGFR immediately post-transplant (difference=-4.22-1.511.20 mL/min/1.73m2, p=0.3). However, ILDKT recipients had faster decline in eGFR per year compared to CLDKT recipients (difference in slope=-1.06-0.76-0.47 mL/min/1.73m2 per year, p<0.001; decline over 5 years for ILDKT=-9.01-7.55-6.10 mL/min/1.73m2 vs. CLDKT=-4.19-3.74-3.29 mL/min/1.73m2).
Conclusion: Patient and graft survival following ILDKT is good through fifteen years post-transplant, supporting this modality, but survival is worse compared to CLDKT recipients. ILDKT recipients bear close monitoring to maximize graft life.
This work was supported by grant numbers K01DK101677 (Massie) and R01DK98431 (Segev) from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Dr. Segev is supported by the K24AI144954 (Segev) from the National Institute of Allergy and Infectious Diseases (NIAID).

right-click to download
