Early clinical complications following HLA-incompatible living donor kidney transplantation
Jennifer Motter1, Kyle R Jackson1, Allan B Massie2, Jacqueline M Garonzik-Wang3, Dorry L Segev2.
1Surgery, Johns Hopkins University, Baltimore, MD, United States; 2Surgery, New York University, New York, NY, United States; 3Surgery, University of Wisconsin-Madison, Madison, WI, United States
Introduction: Incompatible living donor kidney transplant (ILDKT) recipients require desensitization to facilitate transplantation across donor-specific antibody (DSA); however, this substantial upfront immunosuppression may result in higher risk of early complications following surgery.
Method: We compared 682 ILDKT to 5685 compatible LDKT (CLDKT) Medicare-primary recipients drawn from a 25-center cohort with novel linkage to the United States Renal Data System from 1999-2014. We characterized DSA strength as positive-Luminex, negative-flow crossmatch (PLNF, n=129); positive-flow, negative-cytotoxic crossmatch (PFNC, n=349); or positive-cytotoxic crossmatch (PCC, n=204). Diagnoses of deep vein thrombosis (DVT), wound infection, hemorrhage, sepsis, pneumonia, and urinary tract infection (UTI) were ascertained using ICD-9 codes. We used propensity score weighted Cox regression models to quantify the risk of early complications in the first three months, and from three months to one-year post-transplant.
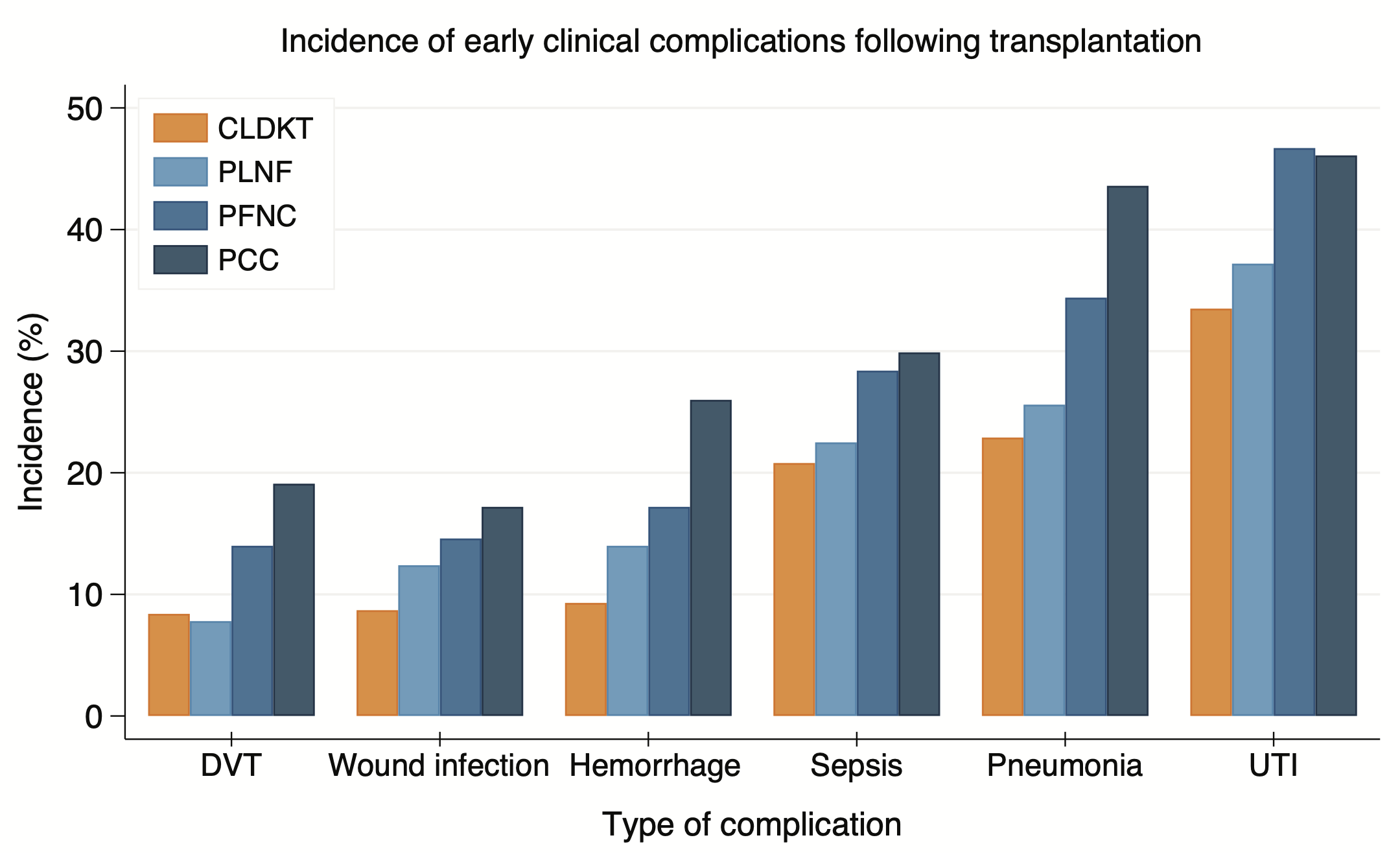
Results: Compared to CLDKT recipients, ILDKT recipients had higher incidence of DVT (14.4% vs. 8.4%), wound infection (15.0% vs. 8.7%), hemorrhage (19.2% vs. 9.3%), sepsis (27.7% vs 20.8%), pneumonia (35.5% vs. 22.9%), and UTI (44.7% vs. 33.5%) (p for all comparisons<0.001) (Figure). Within the first three months, a higher risk of DVT (wHR PLNF=0.050.453.93; PFNC=0.941.793.39; PCC=1.001.883.52), wound infection (wHR PLNF=0.691.232.19; PFNC=1.241.602.06; PCC=0.801.693.62), and hemorrhage (PLNF=1.111.963.47; PFNC=0.911.823.65; PCC=2.072.964.21) were observed across varying levels of DSA strength; however, the risk of these complications decreased thereafter. Although there was no evidence of increased risk of sepsis with the first three months, this risk subsequently increased (PLNF=0.811.874.28; PFNC=0.991.502.30; PCC=1.102.314.81). In contrast, there was higher risk of pneumonia that persisted throughout both time periods (0-3 months wHR PLNF=0.851.914.29; PFNC=1.142.073.75; PCC=1.342.735.59; >3 months wHR PLNF=1.241.571.99; PFNC=0.811.422.49; PCC=1.051.913.48).
Conclusion: Providers should consider these risks during pre-operative counseling, and awareness may aid to improve protocols for ILDKT patient management.
This work was supported by grant numbers F32DK113719 (Jackson), K01DK101677 (Massie), R01DK98431 (Segev), and K23DK115908 (Garonzik-Wang) from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Dr. Segev is supported by grant number K24AI144954 from the National Institute of Allergy and Infectious Diseases (NIAID). Dr. Garonzik-Wang is supported by a Clinician Scientist Development Award from the Doris Duke Charitable Research Foundation.

right-click to download
