A case of cytomegalovirus (CMV) esophagitis without CMV viremia after SARS-CoV-2 infection in a kidney transplant recipient while on CMV prophylaxis
Walaa Dabbas1, Ruchi Naik1, Ignatius Tang1.
1Nephrology, University of Illinois at Chicago, Chicago, IL, United States
Introduction: CMV prophylaxis significantly reduces CMV infection after solid organ transplants, but patient may still present with CMV primary disease or reactivation during the first six months post-transplant. Although high CMV viral load is usually seen in tissue invasive disease, blood CMV PCR my not be able to diagnose gastrointestinal CMV disease as sensitivity of blood CMV PCR is lower in seropositive patients. CMV and SARS-CoV-2 co-infection has been reported particularly in elderly and immunocompromised patients. We report a unique case of CMV esophagitis without viremia diagnosed after recent SARS-CoV-2 infection in a kidney transplant recipient.
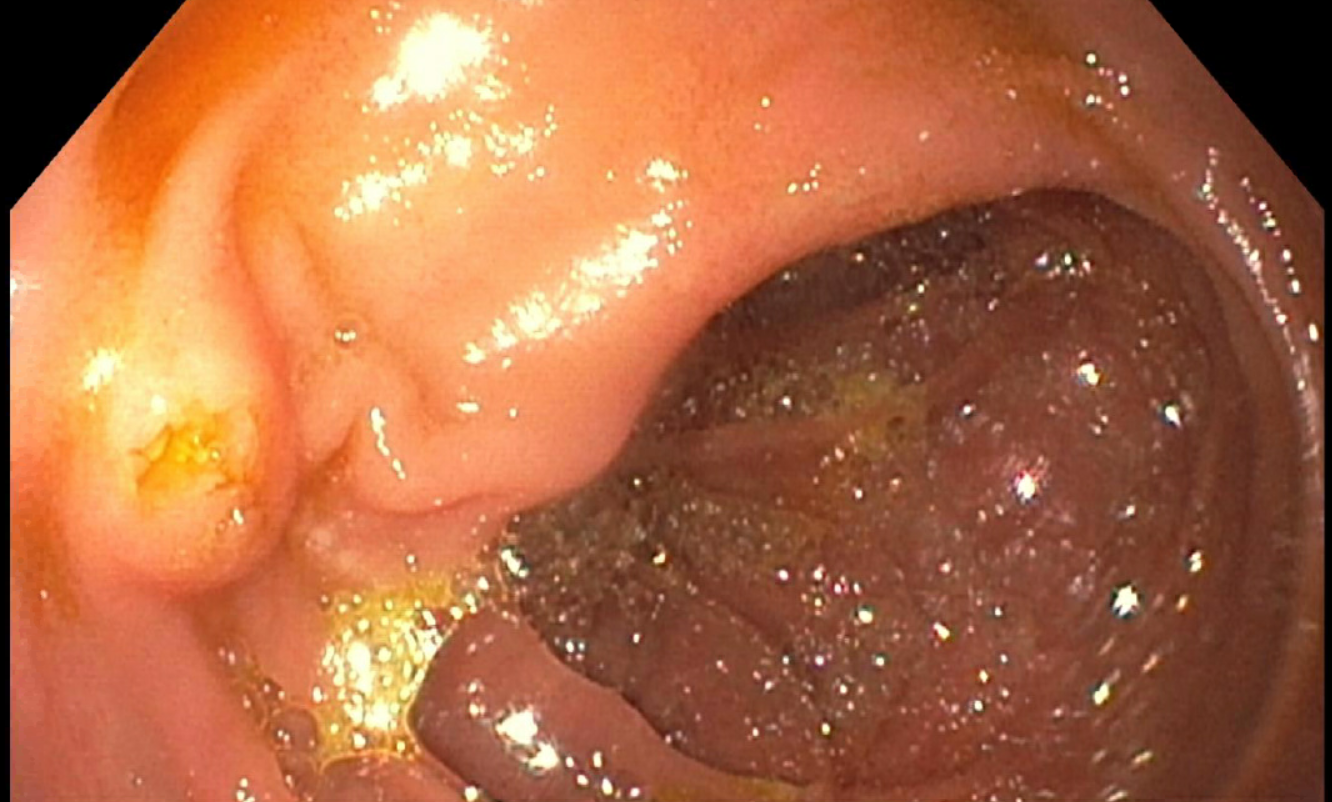
Case: Twenty-eight year old Caucasian female with end stage kidney disease due to unknown etiology received negative crossmatch living related renal transplant from her sister. She received Basiliximab for induction and Tacrolimus and mycophenolic acid as maintenance immunosuppression. Patient had intermediate risk for CMV (Donor CMV IgG negative and recipient IgG positive) and was on Valganciclovir for prophylaxis as per the protocol. She had a stable allograft function with serum creatinine around 1-1.2 mg/dl. She developed SARS-CoV-2 infection with mild respiratory symptoms after 2 months of kidney transplant. Mycophenolic acid was held very briefly, and Prednisone 10 mg daily was added to the regimen. She reported chest pain, nausea and vomiting after resuming mycophenolic acid. Blood CMV PCR was undetectable and other laboratory studies were significant for anemia of 9.3 g/dl (baseline 10 g/dl), with stable renal and hepatic functions, without leucopenia or thrombocytopenia. Upper Gastrointestinal endoscopy revealed a large 4-5 cm circumferential ulceration in the mid esophagus with biopsy features suggesting viral cytopathic effect and rare CMV infected cells. Stomach and duodenum were normal. HSV and fungal stains were negative. Patient was started on oral valganciclovir induction dose and showed symptomatic recovery in a few weeks.
Conclusion: High index of suspicion is necessary to diagnose CMV co-infection and /or reactivation in the settings of SARS-CoV-2 infection and the tissue biopsy is the key for diagnosis of the tissue invasive gastrointestinal disease.

right-click to download
