Quadruple KO porcine adult pancreatic islet induced long-term xenograft survival in diabetic mice
Kyungmin Kwak1, Jae-kyung Park1, Joohyun Shim1, Nayoung Ko1, Hyoung-Joo Kim1, Yongjin Lee1, Jun-Hyeong Kim1, Eui-Hyun Kim1, Pulip Kang1, Jonathan RT Lakey2, Hyunil Kim1, Kimyung Choi1.
1OPTIPHARM Inc, Cheongju-si, Korea; 2Department of Biomedical Engineering, University of California Irvine, Irvine, United States
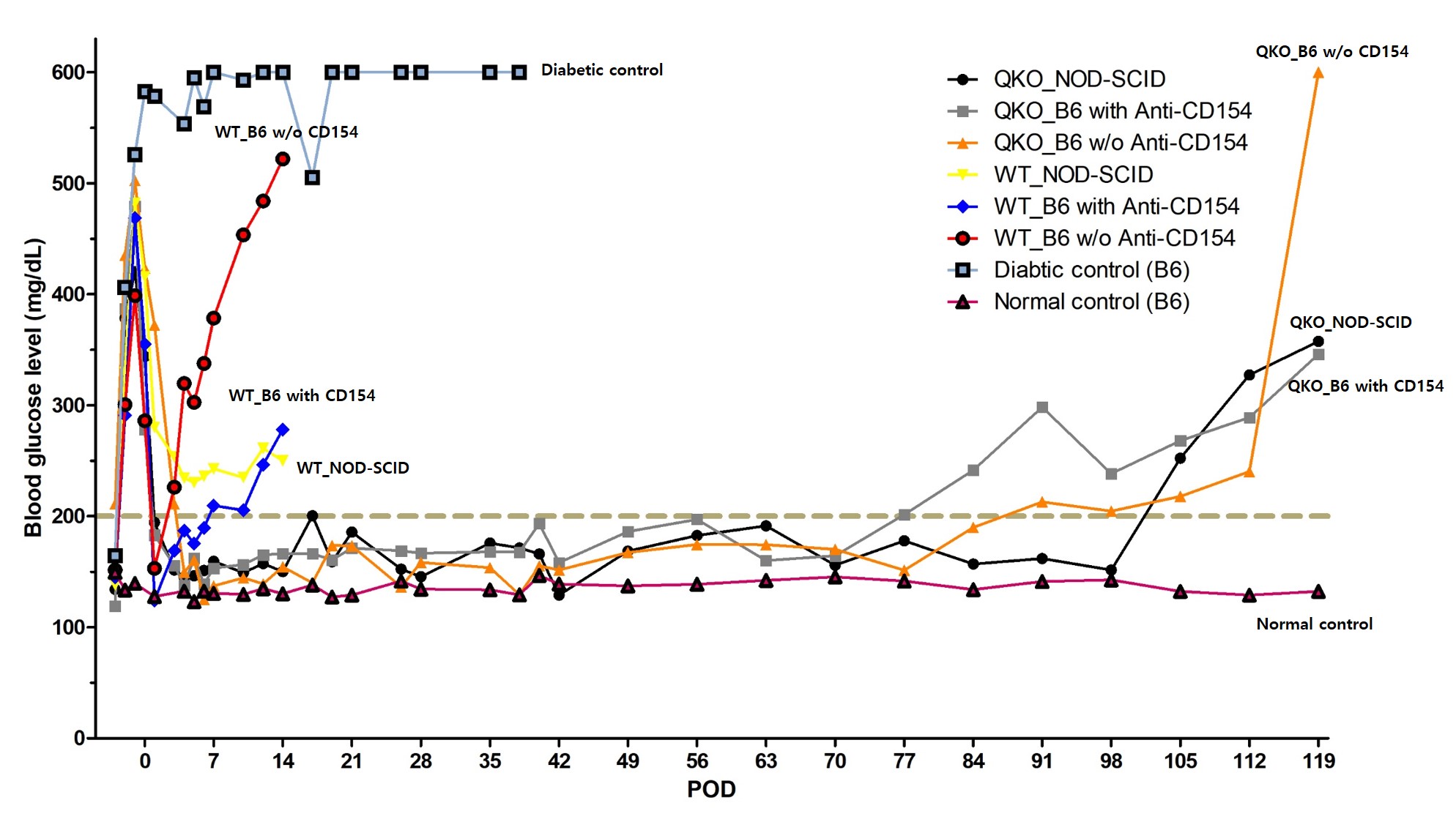
Introduction: Pancreatic islet transplantation has recently emerged as one of the most promising therapeutic approaches for improving glycemic control in Type 1 diabetes patients. However, there were some barriers like deficiency of islet supply due to shortage of pancreas and immune-mediated islet destruction after transplantation. Xenotransplantation using pig is one of the candidate species for clinical transplantation into patients with diabetes. But, some antigen are the obstacle to successful xenotransplantation. For these reasons, we isolated quadruple knockout (GGTA1/CMAH/iGb3s/B4GalNT2 knockout, QKO) islets and transplanted into STZ induced diabetic C57BL/6 and NOD-SCID mice. We identified transplanted QKO porcine islet efficiency in diabetic mice with/without immunosuppressive agent (anti-CD154, MR1).
Methods: Porcine pancreatic islets were isolated from 12 to 18 month old QKO pig using standard enzymatic digestion and purification. Recipients were injected STZ for diabetes induction (160 mg/kg, IP injection). Porcine islet were transplanted into the renal capsule of STZ induced diabetic C57BL/6 and NOD-SCID recipients (n=10 per group). For prevent immune rejection, some recipient groups were treated immunosuppressive agent (anti-CD154, MR1). To compare with QKO islet efficiency, we transplanted WT porcine islet into STZ induced diabetic C57BL/6 and NOD-SCID recipients with or without immunosuppressive agent. We monitored body weight, non-fasting blood glucose level and porcine insulin in serum. Intraperitoneal glucose tolerance test (IPGTT) in POD31 and 123.
Results: Transplantation of QKO and WT porcine islets under the kidney capsule into diabetic mice, hyperglycemia was reversed and became normoglycemia (BGL< 200mg/dL) at day 1. However, the WT porcine islet transplanted group became hyperglycemia within 7 days. On the other hands, QKO porcine islet transplanted group maintained normoglycemia up to 100 days without any immunosuppressive agent (p<0.05 ANOVA). Measured porcine insulin and c-peptide level in serum, normoglycemic mice detected porcine insulin, c-peptide and no mouse insulin was detected.
Conclusion: In this study, we identified that xenotransplantation of QKO islets in diabetic mice improved glucose profile and survival rate in STZ induced diabetic mice. Transplantation of transgenic pig islets could have a significant clinical impact on the treatment of type 1 diabetes. Key islet transplant studies in diabetic primates are currently underway.
Ministry of trade industry and energy, KEIT 20011276, NTIS 1415172664.

right-click to download
