Acute and chronic allograft rejection in the uruguayan lung transplant program in the 2003 – 2022 period
Isabel Villanueva1, Nicolás Tommasino1, Cecilia Chao1, Ana Musetti1, Pablo Curbelo1.
1Lung Transplant National Program, Fondo Nacional de Recursos, Montevideo, Uruguay
Introduction: Lung transplant (LT) is a therapeutic option able to improve the survival and life quality in patients with refractory chronic lung diseases up to maximum treatment. After the first post LT year the major cause of death is the chronic lung allograft dysfunction (CLAD). Acute rejection (AR) has an incidence of 28% in the first year post LT according to ISHLT and increases the CLAD risk. The objective of this article is to describe the events of AR and CLAD in the population of the uruguayan LT program in the January 2003 – March 2022 period.
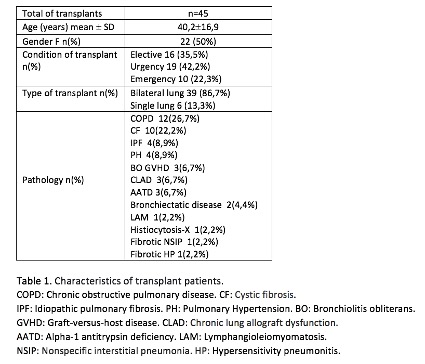
Methods: Descriptive and retrospective study of transplanted and re-transplanted patients.45 transplants were performed, including 3 re-transplants, 6 patients who died due to another cause in the first month after LT were excluded.
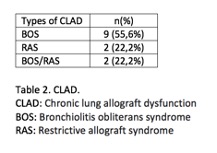
Results: the characteristics of the patients and their transplants are exposed in Table 1. More than half of LT occurred in the last 5 years. The median conditional survival of the program is 7.5 years. There were 29 cellular RA (CAR) events in a total of 19 patients (48.7% of the total); 12 patients presented 1 event, 4 patients 2 events and 3 patients 3 events. These events occurred: 10 in the first month post LT (34,5%), 5 between 1 and 3 months (17,1%), 7 between 3 months and 1 year (24,2%), 7 after the first year (24,2%). Rejection level was A1 in 55,1%, A2 in 41,4% and A4 in 3,5%. The diagnosis was through surveillance endoscopies in 22 events (75,8%), the remaining diagnoses were made in the context of suspected rejection. 23 of the events (79,3%) were asymptomatic, while in the other ones presented as cough, expectoration, and/or dyspnea, being the infectious cause the main differential diagnosis. 17 patients (58,6%) received treatment, 10 cases due to grade of CAR ≥ A2; the remaining patients despite their lower level, presented symptoms, spirometric and /or imageology disturbance, justifing this behavior. Intravenous methylprednisolone were done in 5 patients and oral corticoids in the remaining 12 patients. It is interesting to mention that one patient (2,2%) suffered hyperacute rejection dying 48hs after LT and other one (2,2%) humoral AR. This patient received plasmapheresis and immunoglobin, with satisfactory evolution. 13 patients (44,8%) developed CLAD (Table 2). 9 cases (69,2%) had at least one previous CAR event. 12 of the 13 cases occurred in the first 5 years. All of them had symptoms and functional impairment as presentation form. All received azithromycin and 10 of 13 montelukast. 3 patients were transplanted due to CLAD, 2 developed BOS again.
Conclusion: CAR incidence is comparable to other Latin-American centers but significantly higher than the ISHLT reported. AR is a recognized risk factor for CLAD therefore is necessary to lower the incidence. More studies are needed to know the cause of this high rejection rate reported.

right-click to download
