
Role of the intestinal microbiota in the course of chronic liver disease before and after liver transplantation results of a pilot study
Umid R. Salimov1, Igor O. Stoma2, Aliaksei M. Fedoruk1, Aliaksei E. Shcherba1, Aleksei A. Kovalev3, Oleg O. Rummo1.
1Department of transplantation, Minsk Scientific Practical Center of Surgery Transplantology and Hematology, Minsk, Belarus; 2Chair of Infectious Diseases, Homel State Medical University, Homel, Belarus; 3Chair of Medical and Biological Physics, Homel State Medical University, Homel, Belarus
Introduction: Since the moment the article "Our Other Genome", clearly presenting the genetic catalog of the human gut microbiota, had been published in the journal “Nature”, views of the scientific community on the etiology of chronic liver diseases (CLD) have changed significantly. A large number of recently published studies have been dedicated to the intestinal microbiota in patients with hepatocellular carcinoma (HCC) and alcoholic liver disease as well as the degree of influence of the intestinal microbiota on the course of CLD. However, results of these studies have been quite different. In this regard, we have started our own prospective cohort study of the intestinal microbiota in patients with CLD.
Methods: Our prospective study was based on evaluation of 12 patients suffering from liver cirrhosis and HCC on the background of liver cirrhosis while being on the waiting list for a liver transplantation. Patients were divided into two groups accordingly. In order to determine the gut microbiome palette, the 16s RNA NGS was used. Stool samples were collected 24 hours before, 72 and 168 hours after liver transplantation. The average MELD score within the liver cirrhosis group was 15 (6-30 points). HCC in patients of the second group was within the Milan criteria.
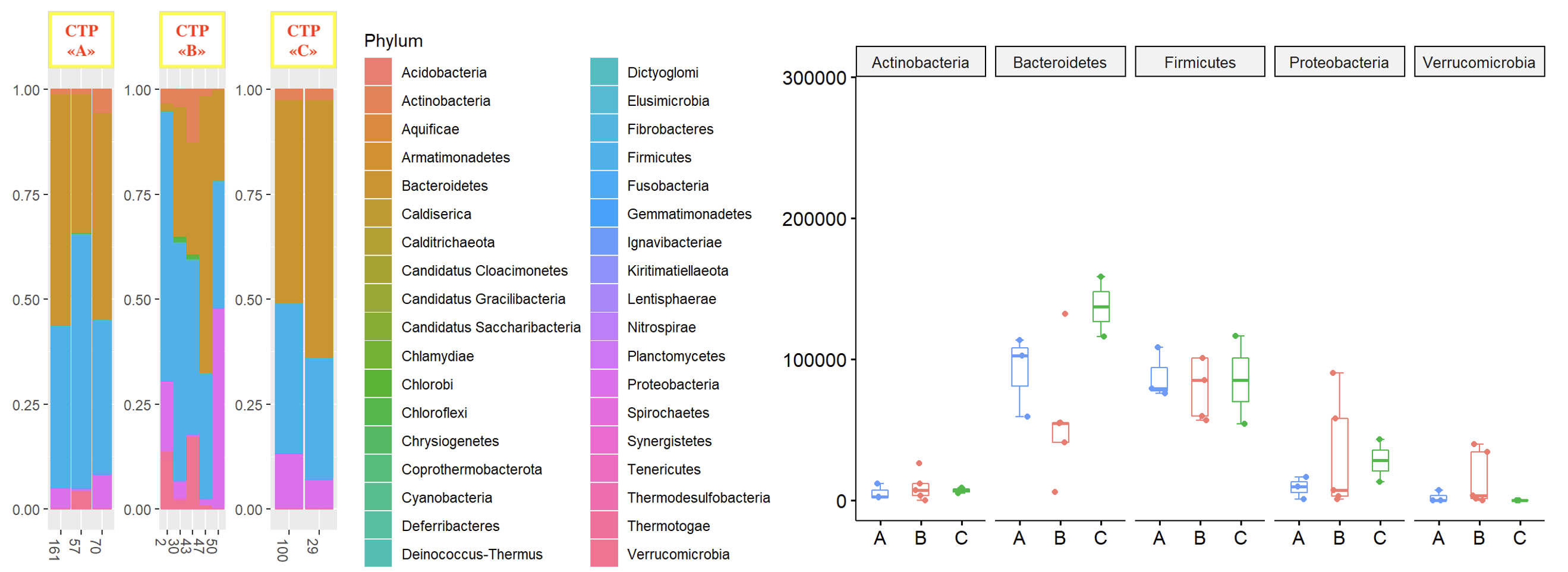
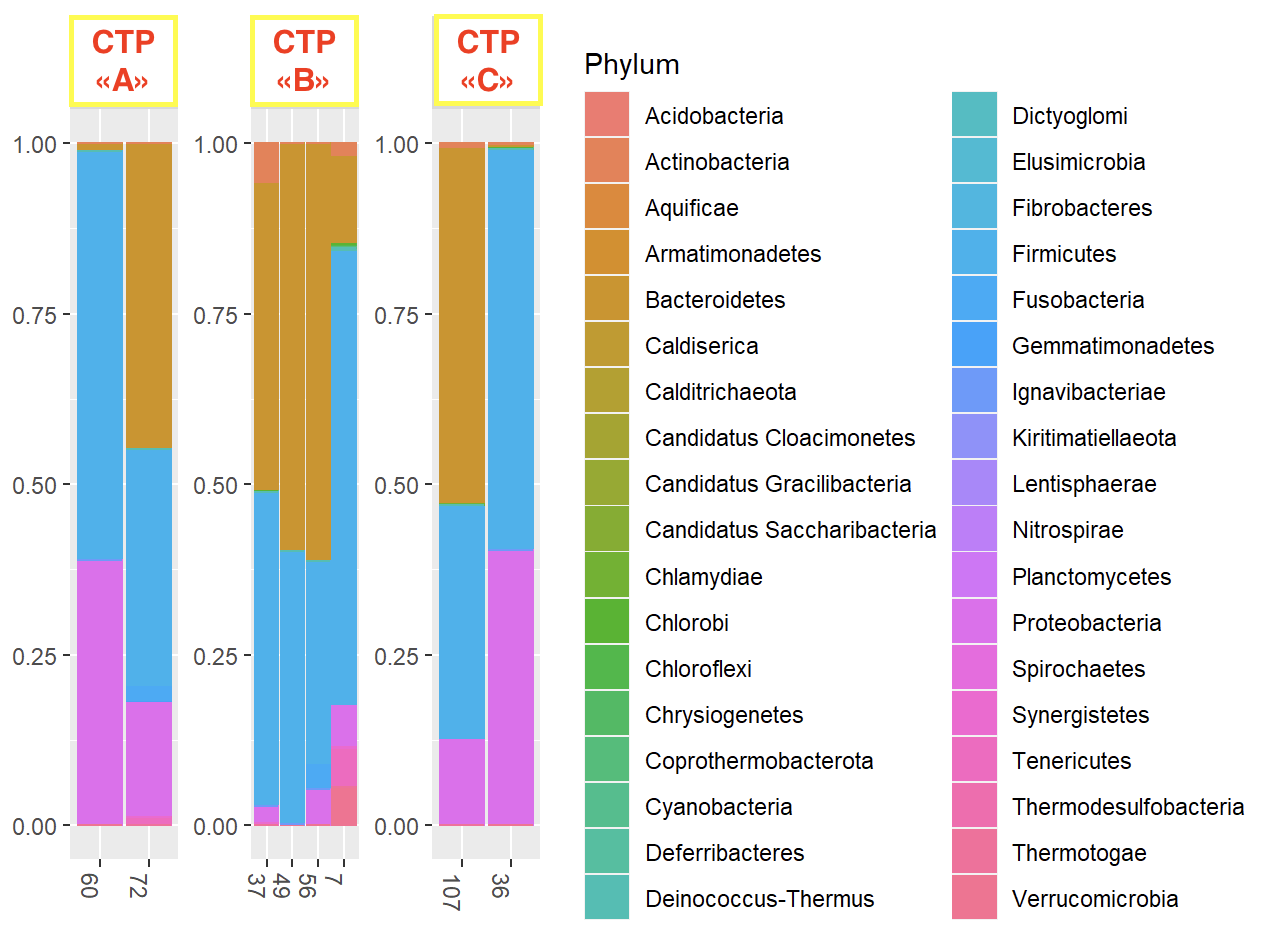
Results: The results of our study showed the absence of any statistically significant difference in the gut microbiota palette of patients with liver cirrhosis of different Child-Turcotte-Pugh functional classes as well as the MELD score (p>0.05) (Fig. 1). Moreover, we did not observe any significant difference in the gut microbiome palette in patients after liver transplantation who were initially referred to different Child-Turcotte-Pugh functional classes (p>0.05). However, in the post-transplant period, Protobacteria were replaced by Bacterioides in patients of the liver cirrhosis group. Besides, in the long-term period after liver transplantation, we noted some difference in the microbiome palette in patients of different functional classes of severity (Fig. 2). At the same time, we noted a pronounced difference in the taxometric picture of the gut microbiom in the post-transplant period in a patient with developed acute cellular rejection.
Conclusion: Since our study was of a pilot nature, its disadvantage may be a small number of studied patients. However, the obtained results indicate the absence of a specific effect of the microbiota on the natural course of liver cirrhosis, even in patients with pronounced liver decompensation (MELD 30). With that said, the revealed microbiome difference in patient with an acute cellular rejection of the graft indicates a dramatically important role of the intestinal microbiota in the development of this complication. In this regard, the obtained data indicate potential significance and expediency of further research in this direction.

right-click to download
