
Born in Lima, Peru, moved to Mexico and graduated from Autonomous University of Guadalajara medical school (UAG). General Surgery by the American British Cowdray Medical Center at Mexico City. Fellowship in Hepatobiliary and Liver Transplant surgery at Hospital Clinic, Barcelona, Spain, Hepatopancreatobiliary and Liver Transplant Surgery at Japanese Red Cross Medical Center, Tokyo and postgraduate training in HPB and Liver Transplant at Asan Medical Center, Seoul, Korea and Pediatric Liver Transplantation at Dr. Juan Pedro Garrahan, Buenos Aires, Argentina.
HPB and transplant staff at Centro Medico Nacional 20 de noviembre-ISSSTE, Head of HPB and Liver Transplant Surgery and Chief of Division until 2022, recently moved to Transplant Division of Hospital Regional Valentín Gómez Farías.ISSSTE, Guadalajara, Mexico. Private practice at Hospital Puerta de Hierro Andares, Guadalajara, leading the adult and pediatric deceased and living donor liver transplantation program. Full Professor of transplant surgery from National Autonomous University of Mexico (UNAM).
Graft versus host disease following liver transplantation: a serious complication
Carlos Florez Zorrilla1, Karina Mendoza Gallo2, Miguel Charco Cruz1, Alberto De Jesus Flores1.
1Liver Transplantation and HPB Surgery, Centro Medico Nacional 20 de Noviembre, Ciudad de Mexico, , Mexico; 2Pediatrics, HGR 89 IMSS, Guadalajara, , Mexico
Introduction: Graft-versus-host-disease (GVHD) after liver transplantation (LT) is a severe complication with high mortality rate (85%). Risk factors, diagnosis and management is challenging. Donor T-lymphocytes play a main role in the immunological attack against the host. We report a case and a comprehensive review of the literature. Around 160 patients are reported in literature with an estimated incidence of 0.5 to 2% of liver transplant. Liver transplantation from hepatocellular carcinoma (HCC) and alcoholic liver disease seems to be the main prevalent diagnosis of patients who developed GVHD.
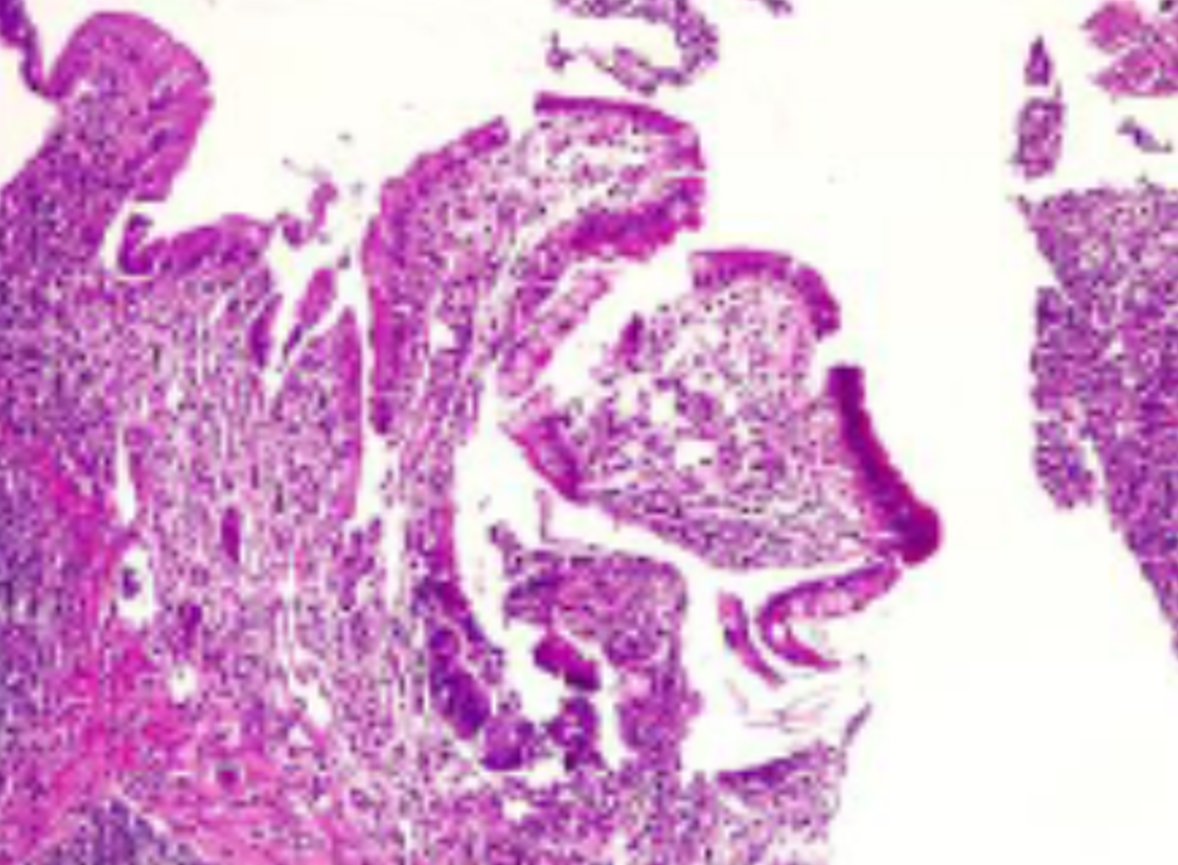
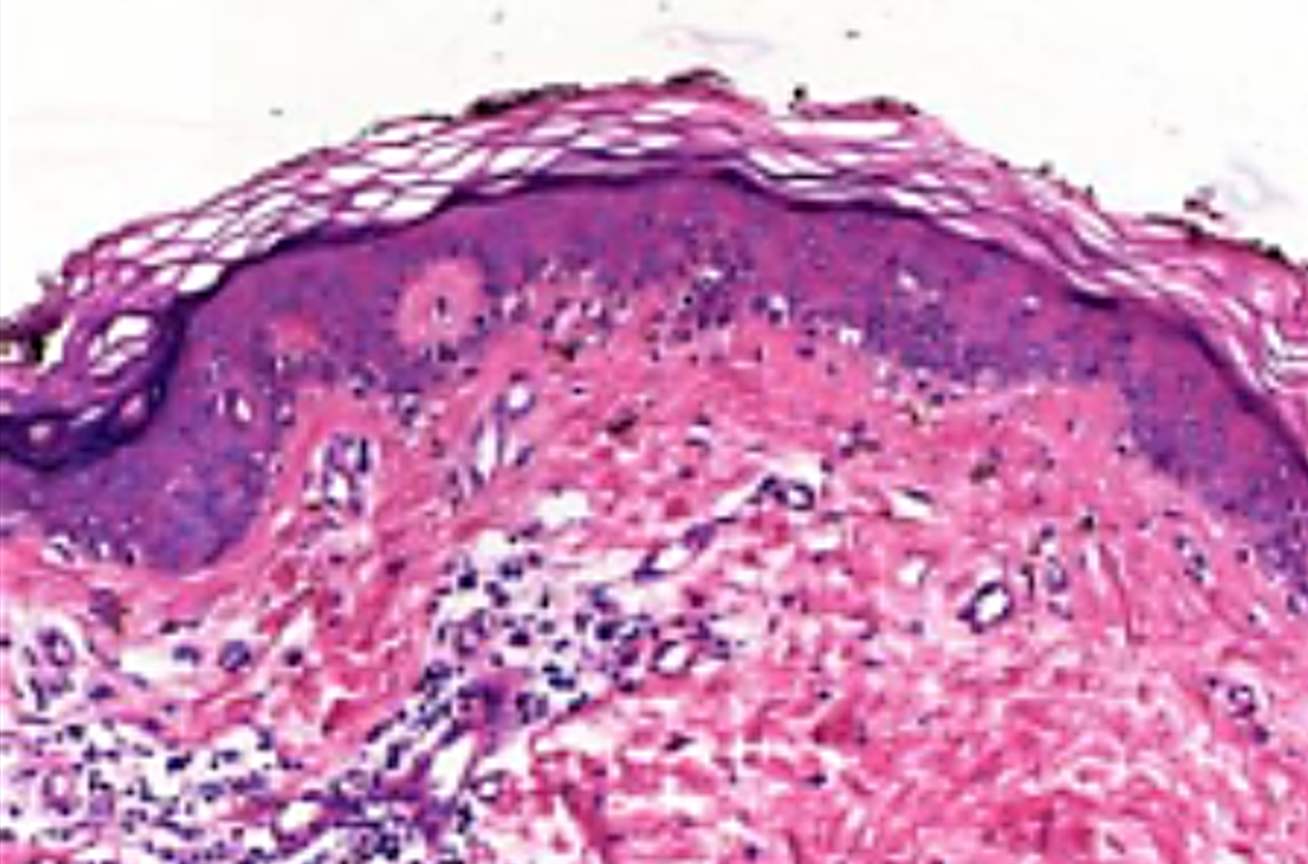
Method: We present a 62-years old male patient with hepatitis C-virus (HCV) cirrhosis and successfully downstaged to Milan criteria HCC. Orthotopic liver transplantation was performed after 6 months of surveillance and discharged uneventfully after 7 days. One month later patient developed abdominal cramps, diarrhea and cutaneous erythema. Mild leukopenia with normal liver and renal function, blood and stool samples were negative, clostridium and other pathogens were also ruled out. Abdominal CT-scan showed moderate distal ileum and colon wall edema. At colonoscopy stellate ulcers was found, biopsy was taken as well to skin lesions. Colon biopsy showed acute inflammation with severe mucosal damage and apoptosis. Skin biopsy showed interphase vacuolar dermatitis. GVHD was suspected and donor lymphocyte chimerism was positive with 5%.

Results: Methylprednisolone was initiated then anti-thymocyte globulin and adalimumab were added. Bacterial, viral and fungal prophylaxis were given. The patient recovered and discharged in good conditions. Five months later the patient developed acute severe pneumonia with extensive lung necrosis that required mechanical ventilation but progressed to refractory respiratory distress and the patient died after 6 months following liver transplantation.
Conclusion: This is the first GVHD case after liver transplantation reported in Mexico. The diagnosis requires a high level of clinical suspicion. There is no strong consensus about the best management, but literature agrees that steroids, IL-2 antibodies, alpha-tumor necrosis factor inhibitors and antibiotics for opportunistic pathogens must be considered.

right-click to download
