
Dr. Luis Eduardo Morales Buenrostro, MD, PhD
Born on June 30, 1971 in Jalisco, Mexico.
Graduate of the Medicine School (1994) at the University of Guadalajara in Jalisco, Mexico.
Postgraduate Training in Internal Medicine (1996-2000) and Nephrology (2000-2003) at the National Institute of Medical Sciences and Nutrition Salvador Zubirán (INCMNSZ) in Mexico City.
Master Degree in Medical Sciences with focus in clinical epidemiology (2004-2006), UNAM. PhD in Medical Sciences with focus in Transplant Immunology (2007-2009), at the National University of Mexico (UNAM) in Mexico City. Research in Transplant Immunobiology at Terasaki Foundation (2007-2008), Los Angeles, CA, USA.
Associated Medical Nephrology at the INCMNSZ (2003 to date) and Head of the Transplant Nephrology program at the INCMNSZ (2008 to date).
Full professor of Transplant Nephrology, UNAM (2013 to date). Associate Professor of Nephrology, UNAM (2005 to date).
Past President of The Instituto Mexicano de Investigaciones Nefrológicas (2013). Past President of the Sociedad Mexicana de Trasplantes (2014-2015). General Secretary of the Sociedad Latinoamericana de Nefrología e Hipertensión (SLANH, 2017-2019). General Secretary of the Sociedad de Trasplantes de América Latina y el Caribe (SATLYC, 2022-2028)
Member of the National Academy of Medicine (2016 to date). Past President of the Mexican Nephrology Board (2021-2022).
National Researcher SNI-CONACYT (2007 to date), currently Level III of III.
Late humoral rejection: will temporality be enough to determine the therapeutic attitude?
Lluvia Marino1, Miguel Maza2, Diana Maldonado2, Luis Morales1.
1Nephrology and Mineral Metabolism, Incmnsz, Cdmx, , Mexico; 2CMN 20 de Noviembre, Cdmx, , Mexico
Introduction: Antibody-mediated rejection (AMR) is the main cause of graft loss, but current guidelines only recommend optimization of immunosuppression in late AMR (>30 days post-transplantation). This study assesses the effectiveness of treatment in late AMR, as well as the responses between clinical rejections and those detected by protocol biopsy.
Materials and Methods: Retrospective cohort of kidney transplant recipients with AMR under follow-up at the INCMNSZ and the “CMN20 de Noviembre”, between January 2011 and March 2021. Chi square and Student's T or Mann-Whitney U were used according to their distribution. Spearman’s correlation was used. A p <0.05 was considered significative.
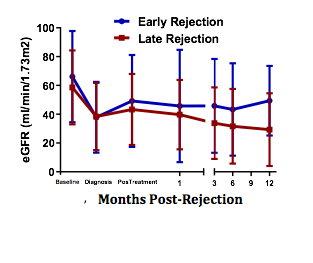
Results: 180 patients were analyzed, 57.2% women, average age 35.9 years, 65.6% living donor, 33% received Thymoglobulin as induction and 66.7% received prednisone, mycophenolate and tacrolimus. 95% were late AMR. 65% detected with protocol biopsy. Class II DSA predominated. The evolution of the glomerular filtration rate (GFR) is shown in figure 1, without difference between early and late AMR. The overall response rate to treatment (GFR maintained or returned within 25% of baseline) immediately, at 1, 6, and 12 months was 73%, 69%, 59%, and 59%, respectively. No difference in GFR for those with and without a response. There was no correlation between the inflammation score (G+ptc) with the GFR in any period. There was an inverse correlation between the chronicity score (ci+ct+cg+cv) and the GFR at diagnosis, at the end of treatment, at 1 and 12 months (-0.261, -0.261, -0.237 and -0.146, respectively).
Conclusions: There were not differences in the response to treatment between early or late AMR and should not determine the therapeutic attitude. Protocol biopsies detected more than half of AMR, demonstrating its relevance.

right-click to download
