Prevalence and risk factors associated with persistent hyperparathyroidism in kidney transplant recipients
Sofia Conci1, Lizeth Fabiola Solano Burgos1, Maria Angelica Rivoira2, Pablo Antonio Novoa1.
1Nephrology and kidney transplant, Hospital Cordoba, Córdoba, Argentina; 2Research in Health Sciences, INICSA-CONICET-FCM-UNC, Córdoba, Argentina
Introduction: Secondary hyperparathyroidism (HPT) is a frequent complication of end-stage chronic kidney disease (CKD). HPT normally remits around the first year after a successful kidney transplant (KT), correcting most of the metabolic abnormalities; however, it persists in 15 to 50%, called Persistent Hyperparathyroidism (pHPT), increasing the risk of loss of bone mass and fractures. Several factors may be associated with development of HPTp, but so far, they are not well defined. In addition, there is no consensus to define the levels of iPTH to establish pHPT. The KDIGO guidelines recommend starting treatment when the iPTH is >100 pg/ml.
Objectives: To evaluate the prevalence of pHPT in the first year after KT and to correlate it with calcaemia (Ca), phosphatemia (P), alkaline phosphatase (AP) and renal function. Evaluate risk factors for the development of pHPT.
Materials and methods: An observational, longitudinal and retrospective study was carried out in patients who received KT from the Nephrology Service of Córdoba´s Hospital between 2010 and 2019. The data were obtained from the medical records of Nephrology Service. Most received induction with basiliximab and an immunosuppressive regimen with calcineurin inhibitors, mycophenolate, and steroids. The variables analyzed were: age of the organ recipient, sex, type of donor, etiology of CKD, the modality and the time on dialysis. The levels of iPTH, Ca, P and AP were recorded at the time of KT, at 6 and 12 months. Renal function was evaluated at 1, 6 and 12 months. Descriptive statistics were used for the analysis. The comparison between the groups was made using the Chi-square test and the t-test, considering p-value <0.05 significant.
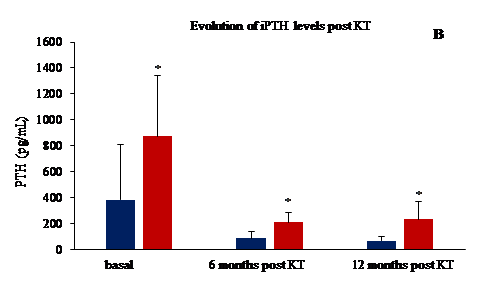
Results: A total of 48 patients were included, the prevalent etiology of CKD was unknown (31%), followed by nephroangiosclerosis (19%). The mean age of the patients was 42.0 ± 11.8 years, 54% were male, 25 patients had PTH before KT (PTH >300 pg/ml, 52%). A total of 10 patients, 20%, most of them women, presented pHPT one year after KT. The longer stay on dialysis (47.9 vs 85.6 months; p<0.01) and the older age of the recipient (40.3 vs 48.7 years; p<0.003) were associated with the development of pHPT. Other risk factors associated with this development were higher levels of AP and iPTH at 6 months post-KT (see Figure 1 A and 2 B). They also presented a propensity for hypercalcaemia (10.5 vs 9.6 mg/dl) and hypophosphatemia (2.5 vs 3.5 mg/dl). One year after of KT, 70% of all patients had GFR between 30-60 ml/min and 30% >60 ml/min, however renal function was similar in both groups.
Conclusion: The most important risk factors for the development of pHPT post-KT were patient's age, time on dialysis, AP and iPTH levels at 6 months post-KT. Resolution of HPT occurred in 80% after one-year post KT. Future strategies should be focus on shortening time in waiting list and the timely treatment of tertiary HPT prior to transplantation.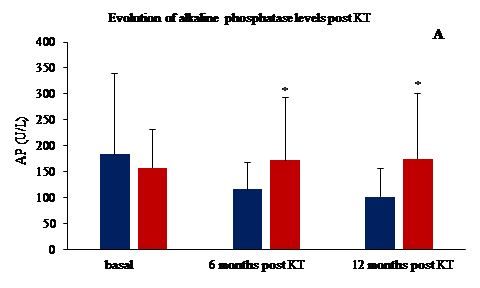

right-click to download
