Main outcomes of pediatric living donor kidney transplantation: a Latin-American cohort
Yenny Baez Suarez1, Andrea Garcia Lopez1, Nasly Patiño Jaramillo1, Fernando Giron Luque1.
1Bogota D.C, Colombiana de Trasplantes, Bogota, Colombia
Background: Renal transplantation in children reduced mortality, improved growth potential, cognitive development, and quality of life. Nevertheless, kidney transplantation in children remains a challenge because of their small size and the scarcity of appropriate allografts. Living-donor kidney transplantation (LDKT) offers higher graft and patient survival rates, and fewer complications compared with transplantation of deceased donors. However, there is a lack of information in Latin-American pediatric kidney transplant patients. Colombiana de Trasplantes has been one of the centers in Colombia that have performed a high proportion of pediatric kidney transplantation from living donors. Therefore, we aimed to evaluate main clinical outcomes, graft, and patient survival for LDKT at our center.
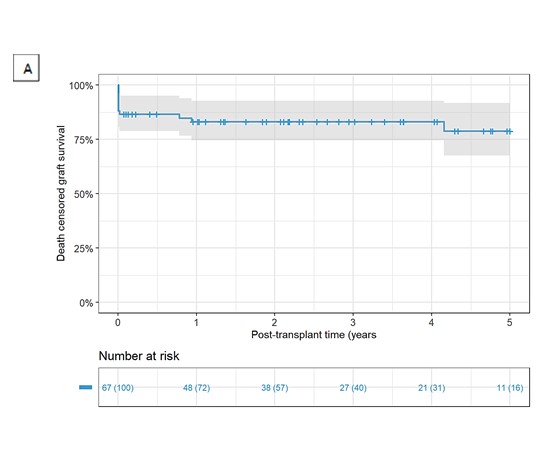
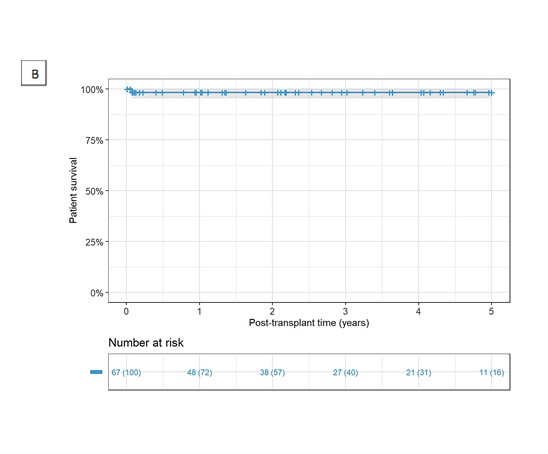
Methods: We retrospectively evaluated a total of 67 LDKT pediatric patients who underwent transplantation form august 2008 to august 2020 at Colombiana de Trasplantes. Graft survival censored for death and patient survival were determined up to 5 years post transplantation by the Kaplan-Meier method. Frequency of thrombosis, hematoma, urinary leak, and reoperation were documented.
Results: A total of 67 LDKT patients were analyzed. Most patients were male (55.2%). The predominant known chronic kidney disease etiology was congenital (n = 24, 35.8%). There were 14 (20.9%) LDKT patients with a preemptive transplant. Dialysis duration was 9.2 ± 13.9 months. Most of the live kidney donors (LKD) were female (n = 39, 58.2%), and relatives for the recipient (n = 61, 91%). Main clinical outcomes were mortality (n =1, 1.5%) and graft loss (n = 14, 20.9%). The graft survival death-censored rates were 83.2% and 78.8% at 1 and 5 years respectively. Patient survival rates were 98.4% at 1 year and was constant during the follow-up. During the follow-up period, a total of 6 patients had vascular complications (8.9%), 1 had peri transplant hematoma (1.5%), 7 had urinary leak (10.4%), and 17 required reoperations (25.4%).
Conclusion: This study describes the experience of 5 years performing LKDT. Our program of pediatric kidney transplantation has achieved optimal patient and graft survival rates with low rate of complications. Since there have been many updates in the field of transplantation, clinical outcomes from a medium-sized center can be noteworthy, although not entirely new.

right-click to download
